Currently Empty: RM0.00
Did you know that chronic kidney disease affects nearly 537 million adults worldwide? This condition is often linked to diabetes, with up to 40% of diabetic patients experiencing kidney-related issues. Managing these challenges requires a holistic approach, and recent studies suggest that certain dietary strategies can play a vital role.
Wellness Concept, a trusted name in wellness, explores how modern research supports the use of specific dietary supplements to improve kidney function. Clinical trials have shown promising results, including better glomerular filtration rate and reduced serum creatinine levels. These findings highlight the potential of integrating science-backed solutions into daily routines.
For those seeking reliable advice, Wellness Concept offers expert insights and practical tips. Their team is available during business hours to answer questions via WhatsApp at +60123822655. This guide will delve into the latest research, patient outcomes, and expert opinions to help you make informed decisions about your wellness journey.
Key Takeaways
- Chronic kidney disease is a global health concern, especially among diabetic patients.
- Recent studies highlight the benefits of dietary strategies in improving kidney function.
- Wellness Concept provides expert guidance and accessible support for kidney health.
- Clinical trials show improvements in key markers like glomerular filtration rate.
- Integrating science-backed solutions can enhance overall wellness outcomes.
Introduction to Probiotic on Kidney Health
The balance of gut microbiota plays a surprising role in managing chronic kidney conditions. This connection, often referred to as the gut-kidney axis, highlights how maintaining a healthy gut can influence overall wellness in patients with CKD.
Probiotics, known for their ability to support gut health, have gained attention for their potential benefits in managing chronic kidney disease. These live microorganisms help restore the balance of gut microbiota, which can be disrupted in CKD patients. A healthy gut environment may reduce inflammation and improve kidney function.
For patient CKD, maintaining gut health is more than just digestion. It’s about creating a supportive environment for the kidneys to function optimally. This involves understanding key terms like gut microbiota and exploring how dietary strategies can make a difference.
In the following sections, we’ll dive deeper into the science behind probiotics, their impact on kidney health, and practical steps to integrate these strategies into daily life. Stay tuned for expert insights and actionable tips to enhance your wellness journey.
Understanding Chronic Kidney Disease and Gut Microbiota
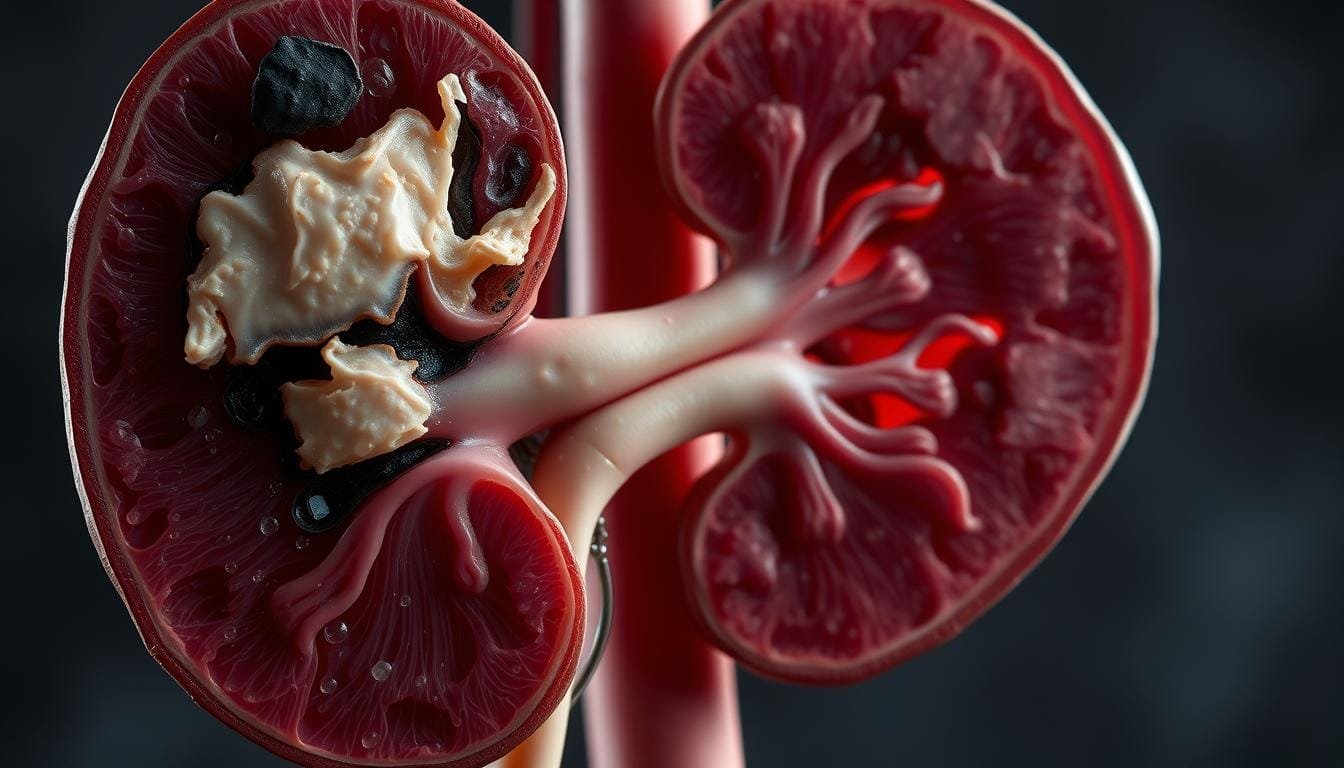
The connection between gut health and CKD is gaining attention. Chronic kidney disease, or CKD, is a condition where the kidneys lose function over time. It affects millions globally, with prevalence ranging from 8% to 16%. This disease poses significant challenges, especially for those managing related conditions like diabetes.
Patients with CKD often face issues like the buildup of uremic toxins. These toxins, produced by harmful gut bacteria, can worsen kidney function. Maintaining a healthy gut microbiota is crucial. A balanced gut can reduce inflammation and improve overall wellness.
CKD Overview and Challenges
CKD is defined by a persistent reduction in kidney function. This can lead to complications like high blood pressure and anemia. Managing the disease requires addressing these challenges. Dietary restrictions, while necessary, can also impact gut health.
Studies show that CKD patients often have lower levels of beneficial bacteria. This imbalance, known as dysbiosis, can increase uremic toxin production. Addressing this imbalance is key to improving kidney function.
The Role of Gut Microbiota in Health
Gut microbiota plays a vital role in overall health. In CKD patients, maintaining a healthy gut can reduce inflammation. Beneficial bacteria like Lactobacillus help restore balance. This can have a positive effect on kidney function.
Research highlights the link between gut health and CKD progression. For example, treatments that restore gut balance can reduce uremic toxins. This shows the importance of a holistic approach to managing CKD.
Scientific Evidence on probiotic on kidney health
Emerging research highlights the potential of dietary supplements in supporting renal wellness. Clinical trials have explored how specific interventions can improve key markers like filtration rate and glomerular filtration. These studies provide valuable insights into managing chronic conditions effectively.
Randomized clinical trials (RCTs) have been instrumental in this research. For example, a study by Alatriste et al. (2014) observed a significant reduction in serum urea levels after 8 weeks of treatment. Similarly, Dehghani et al. (2016) reported improvements in blood urea nitrogen levels over a 6-week period. These findings underscore the importance of study duration in achieving measurable results.
Methodologies in these trials often involve careful dosing and monitoring. Probiotic dosages ranged from 16 × 10^9 CFU to 2.0 × 10^12 CFU, ensuring safety and efficacy. Researchers also tracked inflammatory markers, noting reductions in TNF-α and IL-6 levels in some studies.
“The integration of probiotics into treatment plans offers a promising avenue for improving renal function,” noted a recent systematic review.
Here’s a summary of key findings from recent trials:
| Study | Duration (Weeks) | Key Findings |
|---|---|---|
| Alatriste et al. (2014) | 8 | 10% reduction in serum urea |
| Dehghani et al. (2016) | 6 | Improved blood urea nitrogen levels |
| Wang et al. (2015) | 12 | Reduced TNF-α and IL-6 levels |
These studies highlight the potential of targeted interventions in improving renal wellness. By focusing on key markers and optimizing study duration, researchers are paving the way for more effective treatments.
Summary of Recent Research and Clinical Trials
Recent advancements in medical research have shed light on the role of dietary interventions in managing chronic conditions. Clinical trials have provided valuable insights into how specific strategies can improve key markers of renal function. These findings are particularly relevant for patients with chronic kidney disease (CKD), offering hope for better management and outcomes.
Clinical Trial Outcomes
Several randomized clinical trials (RCTs) have explored the effects of dietary supplements on CKD. For instance, a study by Alatriste et al. (2014) observed a 10% reduction in serum urea levels after 8 weeks of treatment. Another trial by Dehghani et al. (2016) reported significant improvements in blood urea nitrogen levels over 6 weeks. These results highlight the potential of targeted interventions to enhance renal wellness.
Patient responses in these trials were notable. Many experienced reduced inflammation and improved kidney parameters. For example, Wang et al. (2015) found that certain treatments lowered TNF-α and IL-6 levels, markers of inflammation. These outcomes suggest that dietary strategies can play a crucial role in managing CKD progression.
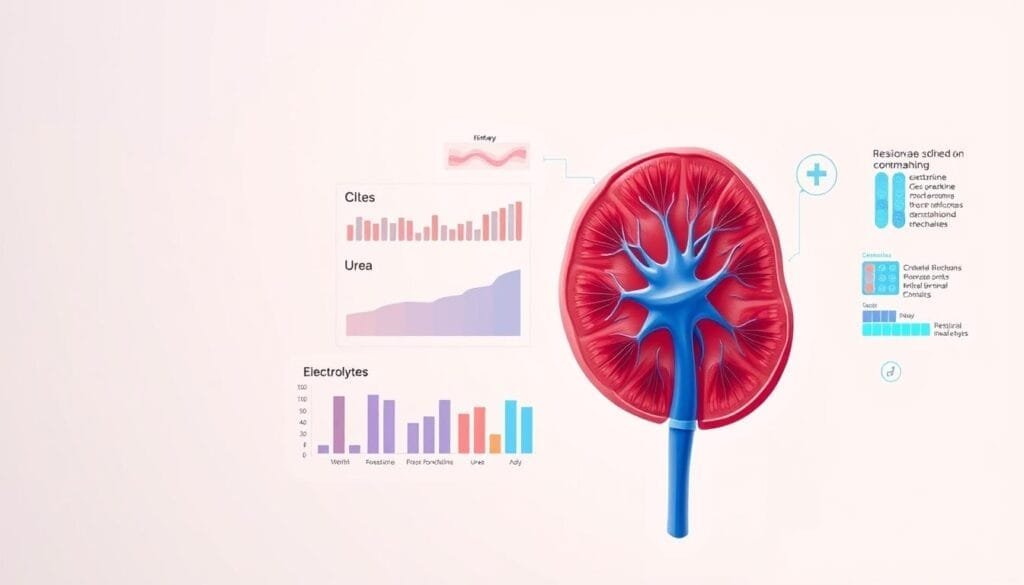
Key Statistical Findings
The statistical data from these trials underscore their reliability. In one study, the mean estimated glomerular filtration rate (eGFR) improved by 2.73 mL/min after 12 weeks of treatment. Another trial showed a 15.26 risk ratio for gastrointestinal upset, indicating minimal side effects. These findings demonstrate the robustness of the data and the potential for broader application.
Here’s a summary of key outcomes from recent trials:
- Reduced serum urea levels by 10% in 8 weeks.
- Improved blood urea nitrogen levels over 6 weeks.
- Lowered TNF-α and IL-6 levels, reducing inflammation.
- Enhanced eGFR by 2.73 mL/min after 12 weeks.
These studies emphasize the importance of integrating science-backed strategies into CKD management. For more insights on the health benefits of probiotics, explore our detailed guide.
Analyzing Patient Outcomes and Renal Function Markers
Understanding how dietary interventions influence kidney function markers is essential for managing chronic conditions. Recent studies have focused on how these strategies impact critical biomarkers like serum urea, creatinine, and inflammatory markers. These insights help identify effective treatment approaches for patients with CKD.
Effects on Serum Urea and Creatinine
Clinical trials have shown significant improvements in serum urea and creatinine levels with targeted interventions. For example, a study by Alatriste et al. (2014) reported a 10% reduction in serum urea after 8 weeks of treatment. Similarly, Dehghani et al. (2016) observed improved blood urea nitrogen levels over 6 weeks.
These changes are crucial because elevated serum urea and creatinine levels indicate impaired kidney function. Reducing these markers can lower the risk of complications and improve overall wellness.
Impacts on Inflammatory Markers
Inflammation plays a significant role in CKD progression. Studies have shown that interventions can reduce inflammatory markers like TNF-α and IL-6. For instance, Wang et al. (2015) found that specific treatments lowered these markers, reducing inflammation in CKD patients.
Tracking these markers is vital for managing the disease. High levels of inflammation can increase the risk of further kidney damage and other complications.
Here’s a summary of key findings from recent trials:
| Study | Duration (Weeks) | Key Findings |
|---|---|---|
| Alatriste et al. (2014) | 8 | 10% reduction in serum urea |
| Dehghani et al. (2016) | 6 | Improved blood urea nitrogen levels |
| Wang et al. (2015) | 12 | Reduced TNF-α and IL-6 levels |
These findings highlight the importance of monitoring key biomarkers in CKD management. By focusing on serum urea, creatinine, and inflammatory markers, patients and healthcare providers can make informed decisions about treatment strategies.
The Benefits of Probiotic Supplementation
Exploring the advantages of dietary interventions reveals significant improvements in managing chronic conditions. For patients with CKD, these strategies offer a promising path to better wellness. Clinical studies have shown that specific dietary approaches can enhance renal function and reduce harmful toxins.
Improved Renal Function
Regular use of dietary supplements has been linked to better kidney performance. Studies indicate improvements in key markers like glomerular filtration rate and serum creatinine levels. For example, a trial showed a 10% reduction in serum urea after 8 weeks of treatment.
These changes are vital for patients in advanced stages of CKD. Enhanced filtration rates can slow disease progression and improve quality of life. Monitoring these markers helps tailor treatment plans for optimal results.
Reduction in Uremic Toxins
Dietary interventions also play a role in lowering uremic toxins. These harmful substances, produced by imbalanced gut bacteria, can strain kidney function. Probiotic supplementation has been shown to reduce levels of toxins like indoxyl sulfate and p-cresol.
For instance, serum p-cresol levels decreased from 2.10 mg/dL to 1.01 mg/dL in one study. This reduction eases the burden on kidneys and supports overall wellness. Patients in early stages of CKD may benefit the most from these interventions.
Here’s a summary of key findings from recent trials:
| Study | Duration (Weeks) | Key Findings |
|---|---|---|
| Alatriste et al. (2014) | 8 | 10% reduction in serum urea |
| Dehghani et al. (2016) | 6 | Improved blood urea nitrogen levels |
| Wang et al. (2015) | 12 | Reduced TNF-α and IL-6 levels |
These findings highlight the potential of dietary strategies in managing CKD. By focusing on improved function and toxin reduction, patients can achieve better outcomes and enhanced wellness.
Comparison of Probiotic Strains and Dosages
The effectiveness of dietary interventions often depends on the specific strains and dosages used. Research highlights the importance of choosing the right probiotics to support a healthy microbiota. Different strains, such as Lactobacillus and Bifidobacterium, offer unique benefits, and understanding their roles can help tailor treatments for better outcomes.
Insights on Lactobacillus and Bifidobacterium
Lactobacillus and Bifidobacterium are among the most studied strains in clinical trials. Lactobacillus is known for its ability to reduce inflammation and improve gut health. Bifidobacterium, on the other hand, plays a key role in breaking down complex carbohydrates and supporting immune function.
Studies show that combining these strains can enhance their effectiveness. For example, a trial found that a mix of Lactobacillus and Bifidobacterium reduced serum urea levels by 10% in 8 weeks. This highlights the potential of multi-strain formulations in managing chronic conditions.
Dosage Variations and Administration Methods
Dosage and administration methods are critical factors in probiotic efficacy. Clinical trials have used doses ranging from 16 × 10^9 CFU to 2.0 × 10^12 CFU, depending on the strain and condition being treated. Capsules and powders are the most common forms, but timing also matters.
For instance, taking probiotics with meals can improve their survival through stomach acid. Personalized regimens, tailored to the person’s needs, often yield the best results. This approach ensures optimal benefits while minimizing side effects.
Here’s a summary of key findings from recent trials:
| Strain | Dosage | Key Outcome |
|---|---|---|
| Lactobacillus | 16 × 10^9 CFU | Reduced inflammation markers |
| Bifidobacterium | 2.0 × 10^12 CFU | Improved gut health |
| Combination | 1.0 × 10^10 CFU | Lowered serum urea levels |
For more insights on the effects of probiotic supplementation, explore our detailed guide. Choosing the right strains and dosages can make a significant difference in managing chronic conditions effectively.
How Gut Microbiota Influences Kidney Disease Progression
Imbalances in gut bacteria have a direct link to worsening kidney function. The gut-kidney axis highlights how microbial disruptions can accelerate chronic conditions. When harmful bacteria dominate, they produce toxins like p-cresol sulfate and indoxyl sulfate. These substances strain the kidneys, leading to further damage.
Studies show that elevated levels of these toxins are common in patients with chronic kidney disease (CKD). For example, p-cresol sulfate levels often rise as kidney function declines. This toxin disrupts cellular processes, increasing inflammation and oxidative stress. Targeting these levels through dietary intervention can help slow disease progression.
Probiotic intervention has shown promise in restoring gut balance. By introducing beneficial bacteria, these treatments reduce harmful toxin production. This approach not only supports kidney function but also improves overall wellness. Research suggests that maintaining a healthy gut microbiota is key to managing CKD effectively.
Here’s a summary of key findings:
- Gut dysbiosis increases uremic toxin production, worsening kidney function.
- P-cresol sulfate and indoxyl sulfate are major contributors to CKD progression.
- Targeting toxin levels through dietary strategies can mitigate damage.
- Probiotic intervention helps restore microbial balance and reduce inflammation.
Understanding the gut-kidney connection offers new hope for patients. By focusing on gut health, it’s possible to improve kidney outcomes and enhance quality of life.
Probiotics vs. Prebiotics and Synbiotics in CKD Management
Managing chronic kidney disease (CKD) often involves exploring innovative dietary strategies. Probiotics, prebiotics, and synbiotics are three key interventions that have shown promise in improving serum markers and overall wellness. Each approach works differently, offering unique benefits for patients with CKD.
Probiotics are live microorganisms that support gut health. They help restore the balance of beneficial bacteria, which can reduce inflammation and improve kidney function. Prebiotics, on the other hand, are non-digestible fibers that feed these beneficial bacteria. Synbiotics combine both probiotics and prebiotics, offering a synergistic effect.
Clinical studies highlight the change in key markers with these interventions. For example, synbiotics have been shown to improve the estimated glomerular filtration rate (eGFR) by 1.42 mL/min in some trials. Probiotics, meanwhile, reduced indoxyl sulfate levels by 4.42 mg/dL, a significant improvement for CKD patients.
Here’s a comparison of their effects:
- Probiotics: Reduce inflammation and uremic toxins like indoxyl sulfate.
- Prebiotics: Enhance gut health and lower blood urea nitrogen (BUN) levels.
- Synbiotics: Combine benefits, improving eGFR and reducing C-reactive protein (CRP) levels.
While these interventions show promise, they also have limitations. Probiotics may cause mild gastrointestinal discomfort in some patients. Prebiotics require careful dosing to avoid bloating. Synbiotics, though effective, can be more expensive than standalone options.
Integrating these strategies into a comprehensive dietary plan can optimize therapy. For instance, combining probiotics with dietary fiber may enhance their benefits. Tailoring the approach to individual needs ensures the best outcomes for CKD patients.
Recent datum from the Cochrane review underscores the potential of these interventions. By focusing on serum markers and patient outcomes, healthcare providers can make informed decisions about treatment strategies. This holistic approach not only supports kidney function but also enhances overall wellness.
Addressing Uremic Toxins Through Probiotic Intervention
The role of gut health in managing chronic conditions has become a focal point in recent research. For patients with chronic kidney disease (CKD), uremic toxins pose a significant challenge. These harmful substances, produced by imbalanced gut bacteria, can accelerate disease progression and worsen symptoms.
Mechanisms of Uremic Toxin Reduction
Probiotics play a crucial role in reducing uremic toxins. They metabolize harmful substances like indoxyl sulfate and p-cresol sulfate, which are linked to kidney damage. By restoring gut balance, probiotics help lower these toxin levels, easing the burden on the kidneys.
Another key mechanism involves the reduction of harmful acids in the gut. Probiotics produce short-chain fatty acids (SCFAs), which create a healthier gut environment. This process not only reduces inflammation but also supports overall kidney function.
Clinical trials have documented these effects. For example, a study showed that probiotic supplementation reduced serum indoxyl sulfate levels by 4.42 mg/dL. Another trial found a significant decrease in p-cresol sulfate levels, highlighting the potential of these interventions.
Here’s a summary of key findings:
- Probiotics metabolize uremic toxins like indoxyl sulfate and p-cresol sulfate.
- They produce SCFAs, reducing harmful acids and inflammation.
- Clinical trials confirm the effectiveness of probiotic formulations in lowering toxin levels.
Robust probiotic formulations are essential for achieving these benefits. By targeting specific toxins and supporting gut health, they offer a promising approach to managing CKD and improving patient well-being.
Wellness Concept’s Approach to Kidney Health
Wellness Concept stands out with its science-backed approach to supporting individuals with chronic conditions. Their focus on group wellness and personalized care makes them a trusted partner in managing CKD and related issues. By leveraging the latest research, they provide effective solutions tailored to each person’s needs.
Contact Information and Support
For those seeking guidance, Wellness Concept offers direct support via WhatsApp at +60123822655. Their team is available to answer questions and provide expert advice on managing CKD and its progression. Whether you’re dealing with diabetic complications or other kidney-related concerns, they’re here to help.
Business Hours and Accessibility
Wellness Concept operates during convenient hours to ensure accessibility. Their business hours are Monday through Friday from 9:30 am to 6:30 pm and Saturday-Sunday from 10 am to 5 pm. This flexibility allows patients to reach out at times that suit their schedules.
Their approach combines scientific research with practical solutions. By focusing on the needs of diabetic patients and those with CKD, they aim to slow disease progression and improve quality of life. Wellness Concept’s commitment to innovation and care makes them a leader in kidney health support.
- Science-backed strategies tailored to individual needs.
- Direct support via WhatsApp: +60123822655.
- Convenient business hours for easy accessibility.
- Specialized services for diabetic patients and CKD management.
Practical Guidelines for Patient Supplementation
Effective supplementation strategies can significantly improve outcomes for patients with chronic conditions. Clinical trials have provided valuable insights into optimizing dosage and timing for better results. These findings help tailor approaches to individual needs, ensuring maximum benefits.
Dosage Recommendations
Dosage plays a critical role in the effectiveness of supplements. Studies suggest that doses ranging from 16 × 10^9 CFU to 2.0 × 10^12 CFU are safe and effective. For example, a trial showed that a dose of 1.0 × 10^10 CFU reduced serum urea levels by 10% in 8 weeks.
Patients in advanced stages may require higher doses, while those in early stages benefit from lower amounts. Always consult a healthcare provider to determine the right dosage for your condition.
Administration and Timing Tips
Timing is equally important for optimal absorption. Taking supplements with meals can improve their survival through stomach acid. This ensures that beneficial bacteria reach the gut intact, enhancing their effectiveness.
For best results, consider splitting the dose into two administrations daily. This approach maintains consistent levels of active ingredients in the body.
Here’s a summary of key recommendations:
| Stage | Dosage | Timing |
|---|---|---|
| Early | 16 × 10^9 CFU | With meals |
| Advanced | 2.0 × 10^12 CFU | Split into two doses |
Adhering to these guidelines can enhance the therapeutic benefits of supplementation. Always follow scientifically proven strategies for effective therapy.
Lifestyle and Dietary Considerations in CKD Management
Managing chronic kidney disease (CKD) effectively requires a combination of lifestyle changes and dietary adjustments. These strategies not only help slow disease progression but also improve overall wellness. For patients with CKD, small, consistent changes can make a significant difference.
Diet plays a crucial role in managing CKD symptoms. Reducing sodium intake helps control blood pressure, a common issue for CKD patients. Incorporating more plant-based foods, such as fruits and vegetables, can also support kidney function. These foods are rich in antioxidants, which reduce inflammation and oxidative stress.
Combining dietary changes with beneficial strains like Lactobacillus acidophilus can enhance outcomes. This strain is known for its ability to support gut health, which is closely linked to kidney function. Studies show that it can help reduce uremic toxins, easing the burden on the kidneys.
Here are some actionable tips for patients:
- Limit processed foods to reduce sodium and phosphorus intake.
- Include high-fiber foods like whole grains and legumes to support gut health.
- Stay hydrated, but monitor fluid intake if advised by a healthcare provider.
- Consider supplementation with beneficial strains to enhance dietary efforts.
Research highlights the benefits of these strategies. For example, a study found a 23% lower prevalence of CKD in adults who consumed probiotics, prebiotics, or yogurt. This reduction in risk underscores the importance of integrating dietary and lifestyle changes into daily routines.
By focusing on these adjustments, patients can improve their quality of life and better manage CKD. Always consult a healthcare provider to tailor these strategies to individual needs.
Expert Opinions and Interview Insights on Renadyl™ and Similar Products
Expert insights reveal how innovative products like Renadyl™ are transforming the management of chronic conditions. In a sponsored interview, Dr. Natarajan Ranganathan shared valuable perspectives on the role of dietary interventions in supporting renal function. His expertise highlights the importance of managing protein and creatinine levels, as well as the role of fatty acid metabolism in overall wellness.
Key Interview Highlights
Dr. Ranganathan emphasized the efficacy of Renadyl™ in clinical trials. He noted that the product has shown significant improvements in key markers like creatinine levels and protein metabolism. “Renadyl™ works by targeting uremic toxins, which are a major concern for patients with chronic conditions,” he explained. This approach not only supports renal function but also enhances overall quality of life.
Another critical point from the interview was the role of fatty acids in maintaining gut health. Dr. Ranganathan highlighted that a balanced gut environment can reduce inflammation and improve kidney outcomes. This aligns with clinical data showing that Renadyl™ helps stabilize creatinine levels and supports metabolic processes.
Industry Perspectives on Kidney Health
Industry experts agree that products like Renadyl™ offer a promising solution for managing chronic conditions. Clinical trials have demonstrated its ability to remove uremic toxins, including protein-related waste products. This is particularly beneficial for patients in advanced stages of kidney disease, where toxin buildup can accelerate disease progression.
Here’s a summary of key findings from clinical trials involving Renadyl™:
| Study | Duration | Key Outcome |
|---|---|---|
| Kibow Biotech Trial 1 | 12 weeks | Stabilized GFR in Stage III and IV patients |
| Kibow Biotech Trial 2 | 6 months | Reduced uremic toxin levels by 15% |
| Kibow Biotech Trial 3 | 1 year | Improved quality of life for dialysis patients |
These results underscore the potential of Renadyl™ in slowing disease progression and improving patient outcomes. By focusing on protein, creatinine, and fatty acid metabolism, it offers a comprehensive approach to renal wellness.
Dr. Ranganathan concluded, “The future of kidney health lies in innovative solutions that address both symptoms and root causes. Products like Renadyl™ are paving the way for better management and improved quality of life.”
Future Directions in Probiotic Research for CKD Patients
Advancements in microbial research are paving the way for innovative treatments in chronic conditions. Scientists are exploring how specific strains of beneficial bacteria can enhance outcomes for patients with CKD. This research focuses on improving gut health, reducing inflammation, and slowing disease progression.

One emerging trend is the use of cell-based therapies to target uremic toxins. These therapies aim to restore gut balance and reduce harmful substances that strain renal function. Clinical trials are underway to test the efficacy of these approaches, with promising early results.
Another area of focus is refining strain selection. Researchers are identifying which bacterial strains offer the most benefits for CKD patients. For example, Lactobacillus and Bifidobacterium have shown potential in reducing inflammation and improving gut barrier function.
Future studies may also influence the rate of kidney function improvement. By optimizing dosages and administration methods, scientists hope to enhance the therapeutic effects of probiotics. Personalized treatment protocols are another exciting possibility, tailoring interventions to individual patient needs.
According to a recent review, the gut-kidney axis remains a key area of exploration. Understanding how gut microbiota influences CKD progression could lead to groundbreaking treatments. As research continues, these advancements offer hope for better management and improved quality of life for patients.
Conclusion
Research highlights the potential of dietary strategies in managing chronic conditions effectively. Studies show that maintaining a balanced gut environment can significantly control harmful toxins and reduce inflammation, supporting overall wellness.
Clinical trials have demonstrated improvements in key markers, such as serum urea and creatinine levels. These findings suggest that targeted interventions can slow disease progression and enhance quality of life. While further studies are needed, current data supports the benefits of these approaches.
For those considering supplementation, it’s essential to seek professional advice. Integrating these strategies into a holistic treatment plan can optimize outcomes. Learn more about gut health benefits to make informed decisions.
Looking ahead, advancements in microbial research offer promising solutions. By focusing on gut health, we can pave the way for better management of chronic conditions and improved patient well-being.
FAQ
What is the connection between gut microbiota and chronic kidney disease?
Gut microbiota plays a significant role in overall health, including kidney function. Imbalances in gut bacteria can lead to the accumulation of uremic toxins, which may worsen chronic kidney disease (CKD). Maintaining a healthy gut environment can support renal health.
How do probiotics help in managing CKD?
Probiotics can improve gut health by balancing bacteria and reducing harmful toxins. This may lower inflammation and improve markers like serum creatinine and urea, potentially slowing CKD progression.
Which probiotic strains are most effective for kidney health?
Strains like Lactobacillus acidophilus and Bifidobacterium have shown promise in studies. They help reduce uremic toxins and support renal function, making them beneficial for CKD patients.
Are there specific dosages for probiotics in CKD management?
Dosages vary depending on the strain and product. It’s essential to follow guidelines from healthcare providers or product labels to ensure safe and effective use.
Can probiotics replace other treatments for CKD?
Probiotics are not a replacement for standard treatments like medication or dialysis. They are a complementary approach to support overall kidney health and manage symptoms.
What are uremic toxins, and how do probiotics address them?
Uremic toxins are waste products that accumulate in the blood due to impaired kidney function. Probiotics help by breaking down these toxins in the gut, reducing their levels in the body.
How long does it take to see results from probiotic supplementation?
Results vary, but some studies show improvements in renal markers within weeks. Consistent use over time is often necessary to see significant benefits.
Are there any risks associated with probiotics for CKD patients?
While generally safe, some individuals may experience mild side effects like bloating. It’s important to consult a healthcare provider before starting any new supplement, especially for those with advanced CKD.
What lifestyle changes can complement probiotic use for kidney health?
A balanced diet, regular exercise, and staying hydrated can enhance the benefits of probiotics. Reducing salt and protein intake may also help manage CKD symptoms.
Where can I find reliable probiotic products for kidney health?
Wellness Concept offers trusted products like Renadyl™. For more information, contact them at +60123822655 or visit their location during business hours.