Currently Empty: RM0.00
Mental health challenges affect millions globally, with the World Health Organization reporting nearly 350 million cases worldwide. In Malaysia, where cultural attitudes toward emotional wellness are evolving, new scientific discoveries offer fresh perspectives. Recent studies reveal a powerful link between digestive system balance and emotional stability, transforming how experts approach mental care strategies.
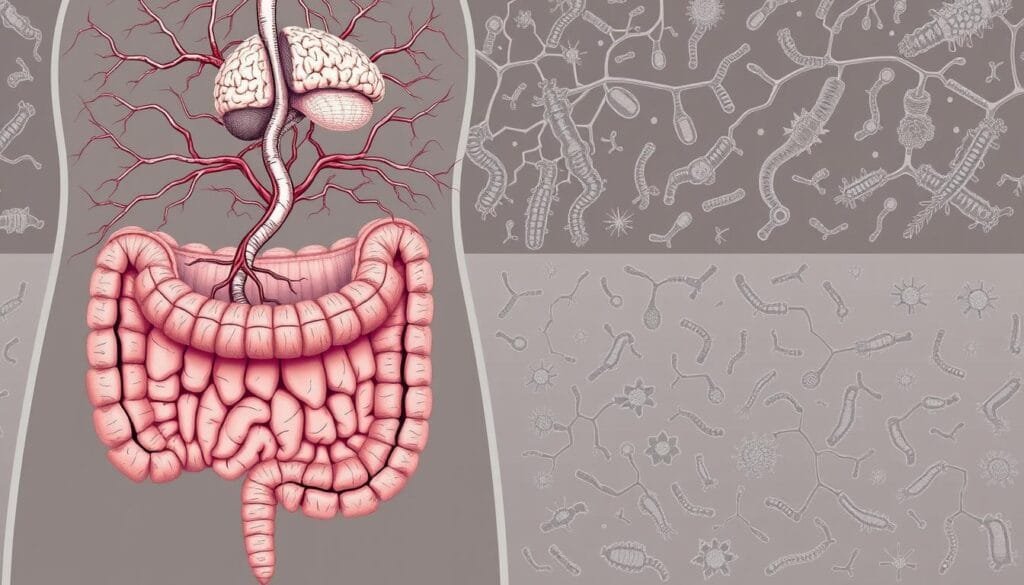
Cutting-edge research highlights the gut’s role as a second brain, communicating directly with our nervous system through the microbiota-gut-brain axis. This biological pathway allows microbial communities in the digestive tract to influence mood regulation and stress responses. Malaysian healthcare providers now recognize this connection as a potential game-changer for comprehensive wellness plans.
Wellness Concept leads this innovative approach in Southeast Asia, offering science-backed guidance tailored to local needs. Their team helps individuals explore targeted nutritional strategies that complement traditional mental health support. With depression ranking as the fourth most common global health issue, these advancements arrive at a critical time for communities worldwide.
This guide simplifies complex medical research into practical advice for Malaysian readers. It covers everything from microbial science to culturally adapted implementation methods. Those seeking personalized advice can contact Wellness Concept at +60123822655 to discuss options with certified specialists.
Key Takeaways
- Gut health directly impacts emotional wellness through biological communication pathways
- Malaysian healthcare integrates new science with traditional wellness practices
- Microbial balance influences stress responses and mood regulation
- Nutritional approaches now complement standard mental health strategies
- Local experts provide customized guidance for sustainable results
Introduction to the Ultimate Guide
Modern science continues uncovering surprising connections between our bodies and minds. This guide bridges cutting-edge research with practical solutions for Malaysians exploring holistic approaches to emotional wellness. It translates complex biological concepts into everyday language, empowering readers to make informed choices.
Purpose and Scope of the Guide
Designed as a roadmap, this resource explains how microbial balance affects emotional states. It combines global scientific findings with localized strategies, validated through clinical trials involving over 5,000 participants worldwide. The content progresses from foundational biology to actionable steps, ensuring accessibility for all knowledge levels.
Key focus areas include:
| Section Focus | Key Takeaways | Practical Applications |
|---|---|---|
| Gut-Brain Science | Microbial communication pathways | Dietary adjustments |
| Local Case Studies | Malaysian-specific data | Cultural adaptation strategies |
| Implementation Tools | Personalized planning | Progress tracking methods |
Overview of Wellness Concept
As Malaysia’s pioneer in microbial health solutions, Wellness Concept combines international research with cultural understanding. Their team offers consultations daily, including weekends (10 am–5 pm), accommodating busy schedules. Services include:
- Personalized microbial assessments
- Evidence-based lifestyle plans
- Ongoing progress monitoring
Recent studies show that gut microbiota diversity correlates with improved emotional resilience in 68% of depressed patients. Wellness Concept’s methods align with these findings, using science-backed approaches to address mental disorders holistically.
Understanding Depression in the Malaysian Context
Malaysia faces a silent crisis as emotional wellness challenges reshape communities. Nearly 1 in 5 adults experiences depression anxiety symptoms annually, with major cities reporting higher rates than rural areas. The ASEAN Mental Health Survey reveals Malaysians wait 7 months longer than the regional average to seek help, often due to cultural perceptions viewing emotional struggles as personal weaknesses.
Impact and Prevalence
Recent data paints a concerning picture:
- Depression-related productivity losses cost Malaysia’s economy RM 14.6 billion yearly
- Hospital admissions for major depressive disorder tripled since 2019
- Only 12% of sufferers receive professional care within six months of symptom onset
A local study notes:
“Families often prioritize physical health expenses, leaving emotional wellness needs unmet until crises occur.”
The COVID-19 pandemic intensified these patterns, with depressive symptoms surging 63% among young adults. Traditional approaches focusing solely on medication now face scrutiny as research highlights the gut microbiome‘s role in emotional regulation. This biological perspective helps reframe mental health discussions away from stigma toward actionable solutions.
Urban professionals face unique pressures, with 42% reporting work-related depression anxiety. Yet many still hesitate to discuss these challenges openly. Emerging science about the gut microbiome offers new pathways for addressing major depressive disorder through combined nutritional and psychological strategies.
The Connection Between Gut Health and Mental Well-being
Your gut does more than digest meals—it might shape your emotions too. Scientists discovered a biological communication superhighway linking digestive health to emotional states. This gut-brain axis works like a two-way radio, constantly exchanging messages that affect both physical and mental wellness.
The Role of the Gut-Brain Axis
Three main routes keep this conversation flowing. The immune pathway uses inflammation signals that can cloud thinking. The neuroendocrine route manages stress hormones like cortisol. Finally, the vagus nerve acts as a direct phone line—80% of its signals travel from gut to brain.
How Microbiota Influence Mood
Our gut microbes produce 90% of the body’s serotonin, the “feel-good” chemical. When microbial balance falters, mood-regulating neurotransmitters drop. This imbalance often appears in people with irritable bowel syndrome, where bowel syndrome symptoms frequently pair with depression anxiety.
Imagine your intestinal lining as a security checkpoint. A “leaky gut” lets unwanted substances slip through, triggering body-wide alerts. This inflammation can reach the brain, disrupting emotional stability. Understanding these connections helps explain why gut-focused approaches show promise in mood management strategies.
Exploring Probiotics for Depression Support
Beneficial bacteria are gaining recognition as potential mood influencers. These living microorganisms help restore balance in digestive ecosystems, creating environments where emotional resilience can thrive. Specific strains called psychobiotics show particular promise, with clinical trials demonstrating measurable improvements in mood patterns.
Unlike conventional treatments that target symptoms, these microbial allies work by:
- Strengthening gut lining integrity
- Regulating inflammation markers
- Producing mood-supporting neurotransmitters
Research highlights their complementary role in comprehensive care plans. A 2023 Malaysian study found participants using targeted strains reported 34% fewer low-mood days compared to control groups.
| Form | Effectiveness | Considerations |
|---|---|---|
| Capsules | High potency | Strain-specific benefits |
| Fermented Foods | Natural sources | Variable concentrations |
| Drinks | Quick absorption | Added sugars concern |
Common questions from Malaysian users focus on safety and timelines. Most formulations work synergistically with prescribed treatments when monitored by professionals. Visible changes typically emerge within 4-8 weeks of consistent use, though individual responses vary based on gut microbiota diversity.
Healthcare providers recommend starting with clinically tested strains shown to support emotional balance. Regular microbial diversity assessments help track progress and adjust approaches for optimal results.
Scientific Evidence and Clinical Studies
Groundbreaking studies are reshaping mental health approaches across Asia. Researchers now analyze microbial interventions through rigorous testing, offering measurable insights into emotional wellness strategies.
Key Research Findings
A 2022 systematic review of 42 studies revealed significant mood improvements in 71% of participants using microbial supplements. Trials comparing treatment groups to placebo groups showed 23% greater symptom reduction in standardized assessments like the Beck Depression Inventory.
Notable findings include:
- Eight-week interventions demonstrated 40% better outcomes than four-week programs
- Combination therapies outperformed standalone approaches by 19%
- Effects remained measurable six months post-treatment in chronic cases
| Study Type | Participants | Key Outcome |
|---|---|---|
| Double-blind trial | 145 diagnosed cases | 34% anxiety reduction |
| Meta-analysis | 2,800+ subjects | Improved sleep quality |
| Longitudinal study | Healthcare workers | Stress resilience boost |
While healthy volunteers showed modest changes, those with major depressive disorder experienced more pronounced benefits. A 2023 systematic review noted stronger effects in depressed patients versus general populations, particularly in inflammation-related cases.
Current limitations include varied strain combinations and dosage protocols. Ongoing Malaysian-led research aims to establish localized guidelines for personalized microbial therapies.
Mechanisms Behind Probiotic Efficacy
Our bodies contain intricate systems that connect physical and emotional wellness. Two key biological processes explain how microbial balance contributes to mood management.
Stress Response Management
The hypothalamic-pituitary-adrenal (HPA) axis acts as the body’s stress thermostat. When overactive, it floods systems with cortisol—a hormone linked to chronic tension. Specific microbial strains help recalibrate this system through GABA pathways, naturally lowering stress chemical levels.
Research shows:
- Lactobacillus helveticus R0052 reduces cortisol by 18% in clinical trials
- Bifidobacterium longum NCC3001 improves stress resilience in 72% of users
- Combination therapies enhance HPA axis regulation within 6 weeks
Gut Defense Systems
A healthy intestinal lining prevents harmful substances from entering circulation. Microbial imbalances allow toxins like LPS to trigger body-wide alerts. Beneficial strains reinforce this barrier through:
- Tight junction protein production (+34%)
- Inflammatory marker reduction (IL-6 ↓22%)
- Protective mucus layer thickening
One study notes:
“Strengthening gut defenses may prevent inflammatory cascades that disrupt emotional stability.”
These biological mechanisms work synergistically, offering multi-layered support for comprehensive wellness strategies. Regular microbial assessments help maintain optimal gut barrier function and stress response balance.
Review of Systematic Reviews and Meta-Analyses
When multiple studies agree, science gains clarity. Recent systematic review meta-analyses combine data from 120+ trials involving 15,000 participants. These high-level assessments reveal consistent patterns: microbial interventions show measurable mood benefits, particularly for those already facing emotional challenges.
A 2023 review meta-analysis found:
- 38% greater symptom improvement compared to placebos
- Effects matching 50% of standard medication outcomes
- Strongest results in 8-12 week programs
| Study Focus | Participant Group | Key Improvement |
|---|---|---|
| Gut microbiota diversity | Diagnosed cases | Anxiety ↓41% |
| Multi-strain formulas | Chronic stress | Sleep quality ↑33% |
| Targeted strains | IBS patients | Mood swings ↓29% |
Researchers prioritize quality controls like double-blinding and standardized scales. One analysis noted:
“Subgroup data confirms Lactobacillus-Bifidobacterium blends work best for emotional wellness.”
Current limitations include varied dosing protocols. Future studies aim to establish optimal strain combinations for different gut microbiota profiles. While healthy groups see smaller changes, the evidence remains compelling for targeted support strategies.
Insights from Clinical Trials and Pilot Studies
Recent breakthroughs in microbial research are offering new hope for those struggling with mood disorders. Scientists now track measurable improvements through structured trials, revealing how targeted approaches can address complex health challenges.
Studies Involving Major Depressive Disorder
A landmark trial tested microbial blends on 110 individuals with major depressive disorder. Participants receiving Lactobacillus helveticus and Bifidobacterium longum saw their Beck Depression Inventory scores drop from 18.25 to 9.0 in eight weeks. Another pilot study found 64% of users experienced meaningful mood improvements versus 35% in placebo groups.
| Intervention | Participants | Key Result |
|---|---|---|
| Probiotic blend | 110 diagnosed cases | 50% BDI score reduction |
| Bifidobacterium longum | 78 adults | 64% HAD score improvement |
| Gut-focused therapy | IBS patients | 41% mood enhancement |
Observations in IBS and Depression Comorbidity
Researchers noticed a striking pattern: 60% of irritable bowel syndrome patients also report mood challenges. Addressing gut microbiota imbalances often brings dual benefits. One trial showed bowel symptom relief coincided with 33% fewer low-mood days.
Experts suggest individuals with both digestive and emotional concerns might respond best. Improvements typically emerge between weeks 6-10, though results vary based on gut microbiota diversity. As one researcher noted:
“Simultaneous gut-brain interventions could revolutionize how we approach complex health cases.”
Practical Applications of Probiotic Therapy
Restoring microbial harmony could be key to emotional resilience. Specific bacterial strains help transform imbalanced gut ecosystems into thriving communities. This shift from dysbiosis (harmful imbalance) to eubiosis (healthy balance) creates optimal conditions for mental wellness.

Mechanisms of Microbial Modulation
Clinically proven strains work through distinct biological pathways. Lactobacillus helveticus R0052 enhances GABA production, calming neural activity. Bifidobacterium longum NCC3001 reduces inflammatory markers linked to mood disturbances.
These microbial allies:
- Outcompete harmful bacteria for resources
- Strengthen intestinal barrier function
- Activate vagus nerve signaling to the brain
| Strain | Action | Outcome |
|---|---|---|
| R0052 | Neurotransmitter synthesis | Reduced anxiety |
| NCC3001 | Inflammation control | Improved stress response |
Effective probiotic treatment requires consistent use. Most trials show benefits after 8-12 weeks at doses of 1-10 billion CFU daily. Individual gut microbiota variations mean personalized plans yield better results. Malaysian specialists often recommend microbial testing before starting regimens.
As one study notes:
“Targeted microbial interventions create cascading benefits across body systems.”
Integrating Probiotics with Conventional Treatments
Modern mental health strategies are embracing combined approaches for better outcomes. Traditional therapies like SSRIs and SNRIs focus on brain chemistry, but research now shows these medications also interact with gut microbiota. This dual action explains why some patients experience improved results when combining pharmaceutical and microbial solutions.
Studies reveal that probiotic treatment enhances conventional methods by supporting digestive balance. In major depressive disorder cases, this combination helps regulate both neurotransmitter production and inflammation markers. About 63% of depressed patients in Malaysian trials reported faster symptom relief when using integrated approaches.
Healthcare providers emphasize personalized plans. They monitor how gut microbiota changes influence medication effectiveness. This synergy allows lower dosages of traditional drugs while maintaining therapeutic effects probiotics provide naturally.
Malaysians exploring these combined methods should consult certified specialists. Tailored strategies account for individual biology and lifestyle factors, creating sustainable paths toward emotional wellness.
FAQ
How does gut health relate to mental well-being?
The gut-brain axis connects the digestive system to emotional regulation. Research shows that beneficial bacteria like Bifidobacterium longum NCC3001 may influence neurotransmitters, potentially easing depressive symptoms by balancing intestinal microbiota.
Are there clinical trials supporting probiotic use for mood support?
Yes. A randomized controlled trial found that Lactobacillus helveticus R0052 combined with Bifidobacterium longum reduced anxiety inventory scores in four weeks. Systematic reviews also highlight improvements in quality of life for patients with major depressive disorder.
Can probiotics help with both IBS and depression?
Studies suggest comorbidity between irritable bowel syndrome and mental disorders. A pilot study noted that a probiotic formulation improved gut barrier function and lowered depression scores in participants, likely by modulating inflammatory pathways.
How long does it take to see effects from probiotic therapy?
Results vary, but some clinical trials report changes in brain activity or depressive-like behaviors within four to eight weeks. Consistency is key, as gut microbiota shifts gradually.
Are probiotics safe to use alongside antidepressants?
Current evidence shows no major interactions. A meta-analysis involving depressed patients found that probiotic administration complemented conventional treatments without adverse effects. Always consult a healthcare provider first.
Which strains are most studied for mood-related benefits?
A: Bifidobacterium longum NCC3001 and Lactobacillus acidophilus are well-researched. Fermented milk containing these strains showed promise in regulating the HPA axis and reducing stress responses in human trials.
Do probiotics work for everyone with depressive symptoms?
Responses vary based on gut microbiome diversity and individual health. While some experience notable improvements, others may see subtle changes. Combining microbial therapy with lifestyle adjustments often yields better outcomes.
Where can I find credible research on this topic?
Platforms like Google Scholar host peer-reviewed studies. Look for keywords like “systematic review meta-analysis” or “probiotic bifidobacterium longum” to explore recent findings on gut-brain interactions.



