Currently Empty: RM0.00
Surprising fact: up to one in ten people report persistent digestive complaints, yet the label many use is not an official medical diagnosis.
Leaky gut is a common phrase in wellness chats across Malaysia, but clinicians use the term differently. Intestinal permeability is a measurable change seen in some diseases such as inflammatory bowel disease and celiac disease.
Many routine gut complaints — bloating, pain, and indigestion — are nonspecific. They can happen without proven increased permeability, so careful evaluation matters before assigning a single cause.
Wellness Concept focuses on clear education and safe, practical steps. They encourage medical assessment when signs persist or worsen and offer local support Monday–Friday 9:30 am–6:30 pm, Saturday 10 am–5 pm. For quick help or bookings, WhatsApp +60123822655.
This guide will explain definitions, how to tell conditions apart, what studies show, which tests lack validation, and low-risk ways to support the gut barrier while evidence evolves.
Key Takeaways
- The phrase many use is not a formal medical diagnosis; intestinal permeability can occur within other diseases.
- Common digestive complaints are often nonspecific and need careful clinical evaluation.
- No single validated home test currently diagnoses this condition; marketed panels have flaws.
- Wellness Concept offers practical education and local support during business hours; WhatsApp +60123822655 for bookings.
- The article will summarize definitions, evidence, testing limits, and safe daily steps to support health.
Understanding increased intestinal permeability today: what “leaky gut” means
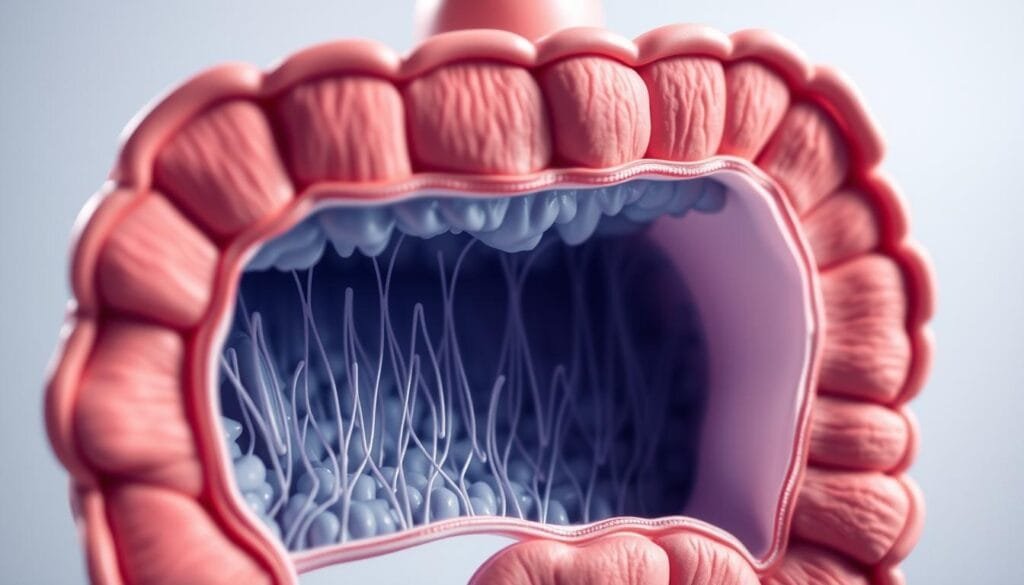
The intestinal lining acts as a selective gate that lets nutrients through while keeping larger particles contained.
How the barrier works: mucus, epithelial cells, and tight junction proteins (claudins, occludin, ZO-1) form a layered intestinal barrier. Secretory IgA and immune cells add protection. A baseline level of intestinal permeability is normal to absorb water and nutrients.
The tight junctions and what can change them
Inflammation, reduced blood flow, or certain medicines can alter tight junctions and raise permeability. The microbiota also influences immune responses and barrier function.
Why the phrase is not a formal diagnosis
Current evidence shows that increased intestinal permeability often appears as a feature of other diseases, such as inflammatory bowel disease and celiac disease, rather than a standalone disorder. Research tools exist but have limits.
| Component | Role | When altered (example) |
|---|---|---|
| Mucus layer | Protects lining from friction and microbes | Thinner after infection or poor diet |
| Tight junctions | Control passage between cells | Changed by inflammation or meds |
| Immune factors (IgA) | Neutralize bacteria and toxins | Altered with microbiota imbalance |
Techniques like lactulose:mannitol testing and confocal laser endomicroscopy are used in research, but limitations prevent routine clinical diagnosis of leaky gut syndrome. For readers in Malaysia seeking friendly explanations, Wellness Concept offers clear guidance. Chat on WhatsApp +60123822655 during business hours if questions arise.
Leaky gut symptoms
A range of everyday digestive complaints leads many to search for a simple explanation.
Typical gastrointestinal complaints people report include bloating, abdominal pain, loose stools or diarrhea, and indigestion. These signs are common across many bowel conditions such as IBS, functional dyspepsia, and SIBO, so they are nonspecific rather than diagnostic.
Non‑specific systemic complaints
Many also describe fatigue, brain fog, or food reactions. Current research shows associations between intestinal permeability and some extra‑intestinal complaints, but it does not prove direct cause-and-effect in most people.
Food sensitivities and allergies can occur, yet adverse reactions are multifactorial. They alone do not confirm a permeability problem.
- Symptoms overlap with other conditions, so self-diagnosis can mislead.
- Researchers find correlations, not definitive proof that permeability causes these complaints.
- Track triggers, timing, and duration to help clinicians assess patterns safely.
Practical note: avoid expensive, unproven tests or extreme elimination diets without guidance. For Malaysians with persistent issues, Wellness Concept offers friendly support — message WhatsApp +60123822655 during business hours to discuss patterns and next steps.
How to identify signs safely: differentiating symptoms from other gut conditions
Distinguishing common digestive complaints from treatable disorders helps people find the right care fast.
Overlap with IBS, functional dyspepsia, and SIBO
Many people with irritable bowel syndrome, functional dyspepsia, or small intestinal bacterial overgrowth report similar issues: bloating, pain, and changes in stool.
These patterns overlap, so a change in intestinal permeability alone does not confirm a single cause.
Red flags that need medical evaluation immediately
Seek urgent care for rectal bleeding, black stools, unexplained weight loss, persistent fever, progressive anemia, severe vomiting, dehydration, or night‑time problems.
Family history of colorectal cancer, celiac disease, or inflammatory bowel disease warrants earlier review.
| Finding | Why it matters | Action |
|---|---|---|
| Rectal bleeding | Could indicate bleeding source or cancer | Urgent medical review and colonoscopy |
| Unintended weight loss | Sign of systemic disease | Blood tests, imaging, specialist referral |
| Night‑time symptoms | Less likely to be functional disorder | Prompt evaluation and testing |
Document diet, stress, medicines, and timelines to help clinicians. Lab tests and imaging may be needed to exclude treatable diseases. For Malaysians unsure how to proceed, WhatsApp +60123822655 during business hours for guidance and referral information.
What studies say about intestinal permeability and disease associations
Scientific studies have mapped higher intestinal permeability in several digestive disorders and explored links beyond the bowel.
Strong evidence shows increased intestinal permeability in inflammatory bowel disease and celiac disease, usually as a feature of ongoing inflammation rather than the original cause.
Some research notes that permeability changes can appear before diagnosis in select conditions, such as type 1 diabetes, but this does not prove causation. Measured bacterial products in blood rise in certain GI and liver diseases, yet their role may be additive rather than primary.
The gut‑brain axis is under active research. Human studies remain limited, so claims linking barrier changes directly to anxiety, depression, or chronic fatigue syndrome are tentative.
- Correlation is frequent; direct causation is rarely proven.
- Animal and early human data need cautious interpretation.
- Practical steps to support the barrier are reasonable while clinicians address proven disease drivers.
For Malaysians seeking a personal read on how these findings may apply, Wellness Concept can help. Chat on WhatsApp +60123822655 or read more about practical approaches at repair your gut lining.
Diagnosis and testing: what’s validated, what isn’t
Accurate diagnosis relies on careful clinical steps rather than a single at‑home panel. No single blood, stool, or urine test can confirm leaky gut or leaky gut syndrome. Many direct‑to‑consumer assays, such as zonulin blood or stool panels, lack consistent correlation with disease.
Common research tools and their limits
The lactulose:mannitol urine test is a research probe of intestinal permeability, but results vary by protocol and interpretation. Confocal laser endomicroscopy gives real‑time mucosal images, yet access and standardisation are limited.
Evidence-based pathways clinicians use
Practitioners prioritise history, exam, and targeted testing to rule out specific disease. Typical steps include:
- basic bloods and inflammatory markers;
- celiac serology and tests for infection or malabsorption;
- selective imaging or endoscopy when red flags appear.
| Step | Purpose | When used |
|---|---|---|
| History & medication review | Identify NSAIDs or antibiotics that affect the barrier | First visit |
| Celiac serology | Exclude celiac disease | When gluten‑related risk exists |
| Endoscopy/biopsy | Direct mucosal assessment | Persistent abnormalities or red flags |
A normal workup may still leave room for supportive lifestyle steps that target overall intestinal permeability. If readers in Malaysia are considering marketed tests, they can message Wellness Concept on WhatsApp +60123822655 for an evidence‑based perspective during business hours.
Root causes and risk factors discussed in research
Certain long-term health issues and lifestyle choices often show up in studies as contributors to increased intestinal permeability.
Chronic inflammation, medications, alcohol, and infections
Ongoing inflammation from chronic diseases can erode the epithelial defences over months or years. This process reduces barrier resilience and raises permeability.
Certain medicines, especially NSAIDs, frequent alcohol use, radiation, and prior gastrointestinal infections also appear in research as factors that can increase intestinal permeability.
Microbiota imbalance and the gut–brain connection
Changes in bacteria communities influence local immunity and tight junction function. Dysbiosis alone does not always cause a problem, but it can contribute when paired with other stressors.
The nervous system affects motility, secretions, and sensitivity via the gut–brain axis. Stress can change these signals and so alter the barrier, though human studies show association more than direct causation for a separate syndrome.
Practical note: the body can repair the intestinal lining when ongoing insults are reduced. For a personalised risk review, Malaysians can message Wellness Concept on WhatsApp +60123822655 during business hours.
| Risk factor | How it affects the barrier | Research note |
|---|---|---|
| Chronic inflammation | Weakens tight junctions and mucus | Common in inflammatory diseases |
| Medications (NSAIDs) | Direct epithelial irritation | Linked to higher permeability in studies |
| Microbiota changes | Alters immune signaling | Often associative, may worsen outcomes |
How to support gut barrier health: practical, low-risk steps
Simple daily habits often influence how well the intestinal lining repairs and protects itself. These steps focus on realistic changes that reduce inflammation and support the barrier without extreme measures.
Nutrition basics: fiber, plant-forward eating patterns, and hydration
Choose a plant-forward diet rich in fiber and microbiota-accessible carbohydrates. These foods feed bacteria that produce short-chain fatty acids, which may help tighten junctions and support the intestinal barrier.
Add fruit, vegetables, legumes, and whole grains slowly to avoid discomfort. Stay hydrated to ease digestion.
Lifestyle levers: sleep, stress management, and physical activity
Regular sleep, stress reduction (breathwork or mindfulness), and moderate exercise support motility and mood. Together, these habits can lower inflammation and help the gut lining recover.
Probiotics and supplements: current evidence, cautions, and safe use
Some probiotics show benefit in specific settings, but no product cures leaky gut syndrome. Start low, go slow, and monitor tolerance. Supplements such as vitamin D, zinc, or glutamine may help as adjuncts under professional guidance.
Foods and patterns that may harm microbiome balance
- Limit ultra-processed food, high-sugar snacks, and high saturated-fat choices.
- Avoid frequent emulsifier-heavy products and many artificial sweeteners when possible.
- Favor diverse, balanced meals over strict elimination unless clinically advised.
Practical help: For Malaysians seeking a tailored plan that fits local food and routines, Wellness Concept offers personalised guidance. Message WhatsApp +60123822655 during business hours for support.
When to seek care in Malaysia and how Wellness Concept can help
Persistent digestive changes deserve a practical check rather than guesswork at home. Timely review helps rule out treatable causes and eases worry.
Personalized guidance for persistent GI concerns
Seek medical review if red flags appear or if issues last more than a few weeks despite basic self-care. Many proposed leaky gut concerns overlap with irritable bowel syndrome and other functional bowel disorders, so a clear plan matters.
Wellness Concept helps Malaysians by tracking patterns, identifying triggers, and preparing focused questions for clinicians. They prioritise evidence-based steps: celiac serology, inflammatory markers, stool tests, or imaging when indicated.
| Finding | Why it matters | Suggested action |
|---|---|---|
| Rectal bleeding | May indicate serious bowel disease | Urgent clinical review and colonoscopy |
| Ongoing change in bowel habit | Could signal infection or inflammatory disease | Blood tests, stool tests, targeted imaging |
| Persistent non‑specific complaints | Often overlaps with IBS or gut syndrome | Structured symptom tracking and nutrition coaching |
Practical care includes focused nutrition and lifestyle coaching, mental well‑being support, and clear referral to hospital care if needed. Safe, steady progress beats quick fixes, especially while evidence evolves.
Message Wellness Concept on WhatsApp +60123822655 for support or appointments. Business hours: Mon–Fri 9:30 am–6:30 pm, Sat 10 am–5 pm, Sun Closed. Continue to the contact section for direct details.
Connect with Wellness Concept: hours and WhatsApp
Wellness Concept makes it simple to know when to reach out for practical, evidence-based support.

The team offers friendly, targeted help for tracking changes, planning nutrition, and reviewing low-risk steps that may help overall health.
Business hours
Monday 9:30 am–6:30 pm
Tuesday 9:30 am–6:30 pm
Wednesday 9:30 am–6:30 pm
Thursday 9:30 am–6:30 pm
Friday 9:30 am–6:30 pm
Saturday 10 am–5 pm
Sunday Closed
Chat on WhatsApp
Reach them on WhatsApp: +60123822655 for quick questions, appointment coordination, or to share updates.
- Know the hours so readers in Malaysia can plan calls and messages.
- Use WhatsApp for brief updates, a symptom diary, or to book a consult.
- The team focuses on practical, low-risk steps that fit Malaysian food and routines.
- If red flags appear, they can advise on timely medical pathways.
- They stress steady habit changes; there are no miracle cures, but a structured plan can improve comfort with gut syndrome or related concerns.
Tip: come prepared with a short food and symptom diary to make each interaction productive. Conversations are friendly, focused, and grounded in current research to guide next steps.
Conclusion
Readers should leave with practical steps that protect the intestinal lining and a realistic view of the evidence.
The current literature shows intestinal permeability is a measurable change in some diseases, but leaky gut syndrome is not an established standalone diagnosis. No single blood, stool, or at‑home panel reliably diagnoses this condition, and unvalidated tests can cause expense and confusion.
Practical actions often help the barrier: choose a fiber-rich, plant-forward diet, sleep well, manage stress, move regularly, and stay hydrated. Reduce ultra-processed food, high sugar, saturated fats, and emulsifiers. Selective probiotics or supplements may help some people, but evidence is mixed and professional guidance reduces risk.
Watch for red flags and seek medical care when inflammation or worrying signs appear. Malaysians can message Wellness Concept on WhatsApp +60123822655 for friendly, research-aware support to turn these ideas into a simple, sustainable plan that may help long-term health.
FAQ
What does increased intestinal permeability mean?
It refers to a change in the intestinal barrier where the lining and its tight junctions allow substances to cross more easily than usual. Researchers study this process to understand links with conditions such as inflammatory bowel disease, celiac disease, and metabolic disorders. Clinicians focus on identifying underlying causes like inflammation, infections, or medication effects rather than labeling it as a standalone disease.
Is “leaky gut syndrome” an official medical diagnosis?
No. Major medical organizations do not recognize it as a distinct diagnosis. Scientists acknowledge that permeability changes occur in several diseases, but the term “syndrome” lacks standardized criteria and validated testing. Health professionals aim to rule out established disorders that explain a person’s complaints.
What common digestive complaints should prompt evaluation?
Symptoms such as bloating, abdominal pain, loose stools, or persistent indigestion deserve medical review. These features overlap with irritable bowel syndrome, inflammatory bowel disease, and small intestinal bacterial overgrowth, so physicians use clinical assessment and targeted testing to find the cause.
Can altered intestinal barrier function cause fatigue or brain fog?
Fatigue and cognitive complaints are non-specific and may coexist with gastrointestinal conditions. Current research shows associations in some populations but does not prove a direct cause-effect link. Providers consider sleep, mental health, metabolic disease, and other contributors when evaluating these complaints.
Are there validated tests to diagnose increased permeability at home or by blood work?
No single at-home kit, blood marker, or routine stool test can definitively diagnose increased permeability for clinical care. Research tools such as the lactulose:mannitol challenge or confocal laser endomicroscopy can assess barrier function in study settings but have practical limits and are not widely used for routine diagnosis.
What clinical tests help rule out other conditions with similar presentations?
Doctors may order blood tests for celiac disease, inflammatory markers, stool studies, breath tests for SIBO, and colonoscopy or imaging when indicated. These evidence-based pathways prioritize ruling in or out established disorders before attributing symptoms to barrier changes alone.
What factors increase the risk of altered intestinal barrier function?
Chronic inflammation, certain medications (for example, nonsteroidal anti-inflammatory drugs), excessive alcohol use, prior intestinal infections, and shifts in microbiota balance are all linked to changes in barrier integrity. Lifestyle and underlying diseases play important roles.
What safe steps can someone take to support their intestinal lining?
Low-risk measures include a fiber-rich, plant-forward diet, adequate hydration, consistent sleep, regular physical activity, and stress reduction. These support overall digestive health and microbiome diversity. Any major supplement or probiotic should be discussed with a clinician to ensure safety and appropriateness.
Do probiotics or supplements fix permeability problems?
Some probiotic strains and nutrients show promise in specific contexts, but evidence varies by product and condition. They are not a universal cure. Clinicians recommend evidence-based use, attention to product quality, and monitoring for benefit or side effects.
When should someone seek urgent medical care for gastrointestinal complaints?
Immediate evaluation is warranted for severe abdominal pain, persistent high fever, bloody stools, unexplained weight loss, signs of dehydration, or any sudden change in mental status. These “red flags” may indicate inflammatory bowel disease, infection, or other serious conditions requiring prompt attention.
How can Wellness Concept help patients with persistent digestive issues in Malaysia?
Wellness Concept offers personalized assessment to investigate symptoms, prioritize evidence-based testing, and create an individualized plan that may include dietary guidance, lifestyle interventions, and coordinated medical referrals when needed. They emphasize safe, practical approaches tailored to each patient’s situation.
What are the clinic hours and how can someone contact Wellness Concept?
Business hours are Monday to Friday, 9:30 am–6:30 pm, and Saturday 10:00 am–5:00 pm. The clinic is closed on Sundays. For support and appointment information, patients can chat on WhatsApp at +60123822655.



