Currently Empty: RM0.00
What people mean by hydrogen water and nerve regeneration often mixes wellness claims with lab findings. This introduction sets a clear purpose: this is a scientific review, not a treatment promise.
Early research shifted thinking about this gas from “inert” to bioactive after key animal reports in 1975 and 2007. That work led researchers to test oral solutions, inhalation, and saline routes.
This piece previews the main themes readers will see: oxidative stress, inflammation, mitochondrial function, and regulated cell death. It also explains why results differ when a person drinks a solution versus inhaling the molecule or using hydrogen-rich saline.
Wellness Concept in Malaysia is noted for local context, but the focus stays on mechanisms, preclinical models (rats, mice), and why caution is needed before applying findings to humans.
Key Takeaways
- This article reviews evidence; it does not make clinical claims.
- Early animal studies changed how researchers view the molecule’s biological effect.
- Main scientific topics: oxidative stress, inflammation, mitochondria, cell death.
- Delivery method matters — oral solutions, inhalation, and saline show different results.
- Most evidence comes from rodent models; human translation needs careful analysis.
Why Nerve Regeneration Matters in Modern Neurorecovery Research
Modern neurorecovery research treats damage as a dynamic biological process rather than a single event. That shift matters because clinical outcomes hinge less on the first mechanical hit and more on what follows.
Primary injury is the instant structural damage: tissue rupture, blood flow loss, and axonal truncation. These changes are often irreversible at the moment of harm.
Secondary injury unfolds over hours to days. Immune activation and microglial responses release proinflammatory mediators such as NO, IL‑1β, TNF‑α, and IL‑6. Neutrophils and monocytes enter the site, driving excitotoxicity, demyelination, necrosis, glial scar formation, and cell death.
How oxidative stress and inflammation block repair
Oxidative stress and reactive oxygen species accelerate tissue loss and limit axon growth. These oxygen species act as damaging factors that worsen demyelination and neuronal loss.
| Phase | Timing | Key features |
|---|---|---|
| Primary | Seconds–minutes | Mechanical damage, blood supply disruption, axon cutting |
| Secondary | Hours–days | Inflammation, ROS release, cytokine surge, glial scar |
| Outcome focus | Short–long term | Structural salvage vs limiting biochemical cascades |
- The spinal cord model is widely used because it shows clear phases and measurable outcomes.
- Many studies aim to limit secondary cascades rather than claim direct regrowth.
- Understanding these responses helps interpret terms like neurorecovery, neurorestoration, and repair.
Hydrogen Therapy in Medicine: From “Inert Gas” to Biological Signaling Molecule
Medical interest grew from a few clear animal findings rather than marketing claims.
Key milestones:
- 1975: a high‑pressure inhalation report showed reduced squamous cell carcinoma in mice, an effect attributed to antioxidant action.
- 2007: a landmark study found that inhaling 2% hydrogen gas selectively scavenged hydroxyl radicals and peroxynitrite, cutting cerebral infarct size in a rat model of ischemia-reperfusion injury.
Researchers began to list this molecule with NO, CO, and H2S as a fourth signaling gas. That label means it may modulate cellular routes, not replace proven treatments.
Most proposed benefits come from shifts in protein activity and pathway signaling. Examples include altered antioxidant enzyme levels and lowered inflammatory transcription factor activity. These changes form the plausible mechanism for observed effects in preclinical work.
| Year | Model | Noted outcome |
|---|---|---|
| 1975 | Mouse (tumor) | Reduced squamous cell carcinoma; antioxidant hypothesis |
| 2007 | Rat (cerebral ischemia-reperfusion) | 2% inhaled gas lowered infarct area; selective radical scavenging |
| Later | Various rats | Mechanistic studies on proteins, enzymes, and oxygen species |
Hydrogen Water and Nerve Regeneration: What the Term Covers Scientifically
Researchers test dissolved molecule, inhaled gas, and saline injection to map exposure and functional changes in models. This section defines those routes and clarifies what “regeneration” means in laboratory studies.
Delivery matters. Drinking a solution delivers low, sustained levels to the gut and blood. Inhalation can raise brain and systemic exposures fast. A saline injection, often called hydrogen-rich saline, gives a direct bolus to injured tissue or circulation.
What “regeneration” means in studies
Authors use several endpoints to claim recovery. Some report behavioral gains: improved movement or sensory scores. Others show tissue findings like axon remyelination or less demyelination on histology.
How outcomes are measured
- Behavioral tests for motor and sensory function.
- Biomarkers of oxidative stress and inflammatory cytokines in tissue or blood.
- Histological measures: cell survival, myelin status, and axon counts.
Reading the claims: stronger evidence combines behavior, biomarker shifts, and histology. Studies that only show short-term biomarker change suggest a biological effect, not full structural regrowth. Careful analysis of methods, route (inhalation hydrogen versus saline injection versus drinking), and endpoints is essential for useful interpretation.
Oxidative Stress, Reactive Oxygen Species, and Neural Injury Cascades
Reactive oxygen species rise sharply after spinal trauma, shifting useful signals into damaging chemistry.
When reactive oxygen becomes harmful
At low levels, reactive oxygen helps normal metabolism and cell signaling. After acute cord injury, production jumps and defenses fail.
This excess triggers prolonged oxidative stress, which damages lipids, proteins, and DNA.
High-impact radical targets
The hydroxyl radical is extremely toxic and lacks any known beneficial role. Peroxynitrite also reacts broadly and worsens tissue loss.
A 2007 report highlighted scavenging these two as a key protective factor in rodent models.
Common markers and downstream cascades
Researchers track markers such as lipid peroxidation (MDA), 8‑OHdG for DNA oxidation, and enzyme shifts like SOD and GSH-Px.
Excess species link to excitotoxicity, demyelination, necrosis, and regulated cell death. Those cascades reduce function after cord injury.
- Markers show biochemical effect even when structural regrowth is not yet proven.
- Understanding these pathways explains why many studies aim to lower oxidative damage rather than claim direct rebuilding of tissue.
Selective Antioxidant Action: How Hydrogen Interacts With Reactive Oxygen Species
Lab data suggest this agent removes highly reactive species while leaving normal cellular signalling mostly intact.

Selectivity describes a targeted neutralization of cytotoxic radicals, such as hydroxyl radical and peroxynitrite, while sparing low-level ROS that support signalling. This idea helps explain why general antioxidants sometimes fail where selective action shows benefit.
Endogenous enzyme responses
Studies reported higher activity of key antioxidant proteins: SOD, CAT, GSH-Px, and HO-1. Increased enzyme expression is often read as bolstered defensive capacity rather than direct tissue repair.
Animal study signals
In rat and mice experiments, inhalation raised SOD activity and lowered markers like MDA and MPO. These biochemical effects correlated with improved behavioral scores in some reports.
- What this means: biomarker shifts support a plausible mechanism.
- What it does not mean: these results are not proof of clinical benefit in humans.
Anti-Inflammatory Effects of Molecular Hydrogen After Injury
After spinal trauma, innate immune cells shift quickly and set a biochemical tone that shapes repair or further loss.
Microglia in the injured cord activate within hours. They release proinflammatory mediators that clear debris but may enlarge the damage zone if unchecked.
How spinal cord injury activates microglia and inflammatory mediators
Early responses include increased expression of nitric oxide, IL‑1β, TNF‑α, and IL‑6. These factors recruit peripheral cells and raise local edema.
Uncontrolled signaling prolongs secondary injury and promotes inhibitory scarring.
Common cytokines and mediators reported
- IL‑1β, IL‑6, TNF‑α — markers of acute proinflammatory activity.
- IL‑10 — an anti‑inflammatory protein that signals resolution.
- MCP‑1, ICAM‑1, HMGB‑1 — chemotactic and adhesion factors that drive cell influx and tissue responses.
Macrophage polarization and tissue repair implications
Macrophages adopt M1 (proinflammatory) or M2 (repair‑associated) states. Earlier M2 skewing reduced bystander damage in healing models.
Studies noted reduced inflammatory factor expression and an earlier M2 profile after exposure, which may favor tissue remodeling.
How lowering inflammation can support regeneration-friendly conditions
Lowering excessive inflammation limits bystander cell loss, reduces edema, and lessens signals that form dense scar tissue. These changes create a more permissive environment for axon sprouting and remyelination in animal work.
Important: shifts in cytokine levels and macrophage markers are mechanistic clues, not proof of a clinical treatment. For more on immune effects in related contexts, see immune system effects.
| Mediator | Typical Role After Injury | What Reduced Expression Suggests |
|---|---|---|
| IL‑1β / TNF‑α | Promote inflammation, fever, cell recruitment | Less secondary tissue loss, lower excitotoxicity |
| IL‑6 / MCP‑1 | Drive acute phase signaling and monocyte influx | Reduced immune cell overload at lesion |
| IL‑10 / M2 markers | Limit inflammation, support repair processes | Enhanced resolution and matrix remodeling |
Mitochondria, Energy Failure, and the Potential Role of Hydrogen
Mitochondria set the pace for recovery because they control energy supply and reactive oxygen output after injury.
Why this matters: mitochondria generate ATP, maintain redox balance, and are the main source of cellular ros during stress. When these organelles fail, cells lose the energy needed for repair and ion homeostasis.
Energy, redox balance, and recovery capacity
Energy failure limits the capacity of injured tissue to restore function. Low ATP halts ion pumps and worsens excitotoxic damage.
Shifts in the NAD(+)/NADH ratio also change metabolic flows and protein activity that guide survival or death pathways.
Reported mitochondrial effects and mechanisms
Preclinical reports link exposure with increased ATP generation and a higher NAD(+)/NADH ratio, which signal improved metabolic resilience.
Researchers also observed markers of mitochondrial biogenesis and protein changes that suggest enhanced organelle health rather than simple antioxidant action.
Mitophagy, PINK1/Parkin, and ischemia–reperfusion contexts
Quality control matters. PINK1/Parkin–mediated mitophagy removes damaged mitochondria after reperfusion injury in animal models.
Studies showed improved inflammatory response and lower apoptosis when mitophagy pathways were engaged, suggesting a plausible mechanism for tissue protection.
“Mitochondrial stabilization can shift outcomes from cell loss to better tissue survival in controlled models.”
- Practical links: mitochondrial protection correlated with lower oxidative stress markers and improved functional scores in rodents.
- Caveat: these are mechanistic, preclinical findings and not confirmed clinical treatments.
Regulated Cell Death: Apoptosis, Autophagy, and Pyroptosis in Nerve Damage
After injury, several programmed cell death routes compete to decide which neurons live or die. Researchers study three main programs to explain tissue loss and possible protection in rodent models and other species.
Apoptosis is tracked by caspase activity and the Bax/Bcl-2 protein balance. Reports showed reduced caspase-3 and caspase-9 levels and lower Bax with higher Bcl-2 expression in treated groups. These shifts favor survival signals and can preserve neuronal circuits.
Autophagy regulation via AMPK/mTOR
Autophagy markers are read through AMPK and mTOR pathway changes. Increased AMPK or lowered mTOR activity often links to enhanced autophagy.
Timing matters: protective autophagy clears damaged organelles early, but prolonged activation can harm cells. Studies report context-dependent effects on cell survival and functional results.
Pyroptosis and inflammasome signaling
Pyroptosis is an inflammatory cell death tied to the NLRP3–caspase-1–GSDMD axis in microglia. Suppressing ROS/NLRP3 signaling reduced caspase-1 activation in cerebral ischemia models, lowering proinflammatory cytokine release.
“Tuning cell death pathways shifts the balance from loss to preservation and can change later recovery potential.”
Why tuning matters: saving vulnerable cells early reduces secondary stress, spares circuits used in movement and sensation, and can improve rehabilitation outcomes in animal models. These mechanistic results point to plausible pathways, but do not claim proven human treatment effects.
| Program | Key readouts | Reported directional change |
|---|---|---|
| Apoptosis | caspase-3/caspase-9, Bax/Bcl-2 | Lower caspase and Bax; higher Bcl-2 expression |
| Autophagy | AMPK, mTOR, LC3-II | AMPK up / mTOR down in protective windows |
| Pyroptosis | NLRP3, caspase-1, GSDMD | Reduced NLRP3–caspase-1 signaling via ROS suppression |
Hydrogen-Rich Saline and Inhalation Hydrogen: What Preclinical Models Suggest
Preclinical teams often compared inhaled gas, saline injection, and drinking routes to see which delivery best changed outcomes after spinal trauma.
Spinal cord injury (SCI) models aimed to preserve tissue, limit secondary cascades, and improve motor scores rather than prove full regrowth. Injury rats and mice showed smaller lesion size and better function in many reports, but these are model‑specific effects.
Why ischemia‑reperfusion models are common
Ischemia‑reperfusion injury reliably creates oxidative spikes and inflammation. That reproducibility helps test whether an intervention lowers reactive damage and inflammatory markers in a controlled setting.
Delivery‑route tradeoffs
- Inhalation gas (often 2%) gave fast systemic exposure and clear dose control in rats and mice.
- Hydrogen‑rich saline injection delivered a local bolus with direct tissue exposure but required invasive injection.
- Oral intake via drinking offered ease and chronic low dosing, yet gave lower peak levels than inhalation or injection.
Across studies, the common message was cautious: saline injection and inhalation produced stronger acute effects in many models, but improved outcomes in rodents do not guarantee similar results in people. Readers should note route differences when interpreting claims about any form of treatment.
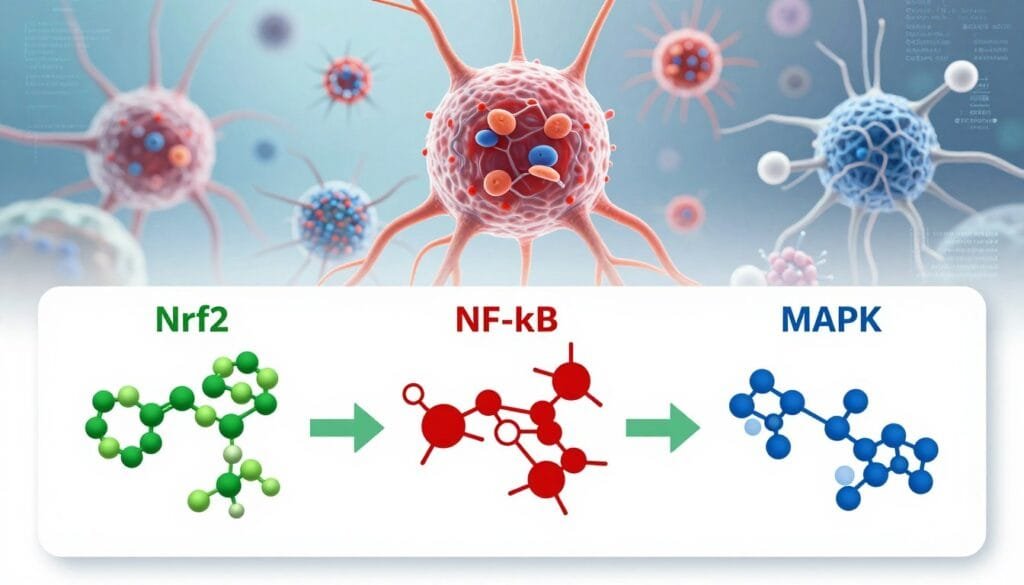
Key Pathways and Biomarkers in the Literature: Nrf2, NF-κB, and MAPK
Key intracellular routes act like control panels that shift cells toward survival or inflammation after injury. In preclinical reports, researchers treat three pathways as primary “switchboards” that explain protective effects: Nrf2/HO-1, NF-κB, and MAPK (ERK, p38, JNK).
Nrf2/HO-1 as an antioxidant defense switch
Nrf2 activation often correlates with higher HO‑1 expression and a stronger antioxidant response. Studies read increased protein expression of this axis as improved resilience to oxidative stress and oxygen‑related damage.
NF-κB as a hub for inflammatory gene expression
NF‑κB controls many proinflammatory genes. Reduced NF‑κB activation in treated groups is used to infer an anti‑inflammatory effect in analysis of treatment models.
MAPK signaling (ERK, p38, JNK) and stress responses
MAPK kinases indicate cell stress and fate decisions. Researchers measure phosphorylation ratios of ERK, p38, and JNK to show pathway modulation after injury.
How pathway readouts support mechanism claims
Pathway shifts—phosphorylation changes or altered protein expression—offer mechanistic clues. However, claims gain weight only when these shifts match behavioral outcomes, histology, and consistent biomarker improvements.
“Pathway readouts are supportive evidence, not standalone proof of treatment success.”
Neuropathic Pain Evidence: Hydrogen Water in a Partial Sciatic Nerve Ligation Mouse Model
This preclinical study followed mice for 21 days to capture early and later phases of pain after partial nerve injury. The Kawaguchi et al. (2014) study used a C57BL/6 PSNL model to compare treated and control groups.
Design and behavioral measures
The study recorded mechanical allodynia with the von Frey test and thermal hyperalgesia with the plantar test. Tests repeated over day 0–21 allowed clear tracking of induction versus maintenance phases.
Timing effects and results
During day 0–4 both mechanical and thermal thresholds improved in the treated group. From day 4–21 thermal sensitivity remained better, while mechanical allodynia returned toward control levels. These timing differences suggest the strongest benefit occurred early after injury.
Tissue markers and practical details
Markers of oxidative stress—4‑HNE and 8‑OHdG—dropped in the spinal cord and dorsal root ganglion. Treated mice drank from aluminum bottles that were exchanged daily to keep hydrogen levels >0.6 mM in the water.
Takeaway: this mouse study shows reduced oxidative stress and improved pain‑like behavior in a PSNL model, but the authors present these findings as mechanistic preclinical evidence, not proof of clinical therapy.
Beyond Nerves: Wound Healing Findings That Inform Regeneration Biology
Skin repair models highlight shared rules that shape any successful healing response. These studies focus on how inflammation control, scaffold building, and new blood vessels create a permissive environment for recovery.
Key preclinical findings from a high-concentration 66% exposure model reported roughly a threefold faster closure by day 11. The treated group showed earlier re-epithelialization, quicker extracellular matrix (ECM) deposition, and more robust vascular signals.
ECM, collagen dynamics, and structural support
Early deposition of collagen I, III, and XVII provided a scaffold that supported tissue strength and remodeling. Faster ECM formation can reduce wound gape and guide organized repair.
Epidermal stem cell activation and vascular changes
Researchers saw earlier epidermal stem cell proliferation followed by timely differentiation. This sequence favored barrier restoration while new capillaries improved oxygen delivery and nutrient flow.
How these findings relate to other repair contexts
Shared mechanisms—inflammation tuning, mitochondrial maintenance, and matrix timing—appear across tissue types. Those common themes matter when researchers consider what makes a microenvironment supportive of cell survival and growth.
“Repair-friendly tissues balance inflammation, scaffold formation, and blood flow; changing one element alters the whole process.”
| Feature | Reported change | Why it matters |
|---|---|---|
| Re-epithelialization | ~3× faster by day 11 | Faster barrier restoration and lower infection risk |
| ECM/collagen (I, III, XVII) | Earlier deposition | Improved structural support and remodeling |
| Epidermal stem cells | Earlier proliferation, later differentiation | Coordinated renewal and durable closure |
| Vascularization | Increased capillary signals | Better oxygenation and nutrient delivery |
Authors noted reduced systemic Th1/Th17 inflammation and linked benefits to preserved mitochondrial function rather than antioxidant action alone. Still, these wound results do not prove direct repair of other tissues. They do, however, offer useful mechanistic clues.
For a related discussion on skin outcomes and collagen, see this comparison on hydrogen vs collagen for skin.
What Current Studies Do and Don’t Prove About Treatment in Humans
Preclinical findings offer mechanism clues, but they stop short of confirming human benefit. Most supportive evidence came from controlled lab models and animal groups, where dosing, timing, and injury type were tightly managed.
Why models may not map directly to clinical care. Animals are useful for mechanistic analysis, yet human injuries vary in location, severity, and day-to-day timing of intervention. That heterogeneity changes how a therapy performs outside the lab.
Common limitations appear across reports. Dosing differs by route (inhalation, saline injection, oral intake), study duration varies by day endpoints, and results often mix biomarker shifts with functional measures. Readers should note which was measured.
How to read results responsibly
Look for reproducibility across multiple studies and models rather than a single positive group. Ask whether an effect was a short-term biomarker change or a durable functional gain.
“Positive lab signals guide research, not clinical practice.”
Practical note: in wellness settings in Malaysia, treated use of this approach should be framed as evolving support, not a replacement for standard medical care or rehabilitation.
Practical Considerations for Hydrogen Water Use in Wellness Settings
Practical use in a wellness setting hinges on handling, dose maintenance, and clear expectations about what the product can reach in the body.
Stability and concentration: Lab work kept levels >0.6 mM by storing solution in sealed aluminum bottles and exchanging them daily. Readers should note that concentration falls quickly if bottles are open or stored in warm light.
Route expectations: Drinking a solution gives low, sustained exposure aimed at general systemic effect. By contrast, inhalation gas raises peak exposure fast, while saline injection delivers a local bolus to tissue. These routes are not interchangeable for targeting specific sites.
Safety framing: Research reports the agent selectively targets cytotoxic radicals and shows no known noxious metabolites in controlled studies. That said, “safe in studies” does not equal a clinical treatment claim.
Questions to ask providers: How is concentration measured? Where and how are products stored? Which study results support the service? Wellness Concept can help Malaysian readers learn more without making medical promises.
Wellness Concept Malaysia: Visiting Information for Readers Who Want to Learn More
Readers in Malaysia often need clear, local access details to turn research curiosity into an informed visit. This short guide lists weekly availability and practical talking points so groups or individuals can plan a visit without extra searching.
Business hours and weekly availability
Monday
9:30 am–6:30 pm
Tuesday
9:30 am–6:30 pm
Wednesday
9:30 am–6:30 pm
Thursday
9:30 am–6:30 pm
Friday
9:30 am–6:30 pm
Saturday
10:00 am–5:00 pm
Sunday
Closed
Wellness Concept frames this article as a scientific review. Visitors should come to learn about the research rather than expect guaranteed clinical outcomes.
Helpful questions to bring when discussing hydrogen use and water handling:
- How is concentration measured and recorded on site?
- How are products stored to preserve levels and stability?
- Which studies support expected short‑term biomarker changes versus lasting clinical results?
The team recommends booking during weekday hours for group visits and allowing time to review methods and published findings. Wellness Concept staff will answer procedural questions and point to the original studies used to inform services.
Conclusion
This review ties consistent lab signals into a clear takeaway about biological conditions that favor recovery after injury. ,
Most preclinical work showed control of oxidative stress, modulation of inflammation, better mitochondrial function and adjusted cell‑death signaling as the likely mechanism for observed protective effects. Those shifts reduced biomarker damage and improved behavior in models.
A concrete example is the PSNL mouse study where hydrogen water correlated with lower oxidative stress markers in spinal cord and DRG plus reduced pain‑like behaviors. Wound healing reports add support for repair‑friendly biology, not direct tissue rebuilding.
Readers should seek human clinical evidence, clear dosing methods, reproducible endpoints and independent analysis before treating this as a validated therapy. For practical next steps in Malaysia, consult the Wellness Concept visiting guide for evidence‑based discussion.
FAQ
What is the basic idea behind molecular hydrogen as a therapeutic agent?
Molecular hydrogen acts as a selective antioxidant that neutralizes highly reactive oxygen species like hydroxyl radicals and peroxynitrite, while sparing signaling ROS needed for normal cell function. Preclinical work in rodents shows modulation of oxidative stress, inflammation, and cell-death pathways after injury, which may create a tissue environment more favorable for repair.
How does this approach differ by delivery route — inhalation, hydrogen-rich saline, or dissolved gas in drinking fluid?
Delivery routes change onset, dose control, and tissue exposure. Inhaled gas achieves rapid systemic levels useful for acute models such as ischemia-reperfusion. Hydrogen-rich saline provides a parenteral option with controlled local dosing in animal studies. Dissolved gas in drinking fluid or bottled solutions gives lower, prolonged exposure that may suit wellness or chronic models. Each route shows different practical trade-offs in experiments.
What outcomes do researchers use to judge "regeneration" in nerve studies?
Studies use behavioral recovery (motor scores, sensory thresholds), histology (axon counts, remyelination), electrophysiology (conduction velocity), and biomarkers (oxidative markers, inflammatory cytokines). Effective reconstruction usually requires improvement across multiple readouts rather than a single metric.
Which reactive oxygen species are most relevant to neural injury, and why?
Hydroxyl radicals and peroxynitrite are highly cytotoxic and damage lipids, proteins, and DNA. Superoxide and hydrogen peroxide function in signaling but can contribute to harm when unchecked. Targeting the most destructive species while preserving signaling ROS is key in many studies.
What anti-inflammatory effects have been reported after treatment in spinal cord or peripheral nerve models?
Experimental reports show reduced microglial activation, lower levels of IL-1β, IL-6, TNF-α, MCP-1, and HMGB1, and sometimes increased IL-10. Shifts in macrophage polarization toward tissue-repair phenotypes are also described, which supports a microenvironment permissive to regeneration.
Are there clear mitochondrial benefits shown in preclinical work?
Several rodent studies report improved mitochondrial function markers — better ATP production, maintenance of NAD+/NADH balance, reduced mitochondrial ROS, and indicators of preserved mitochondrial biogenesis. These effects link to reduced energy failure after ischemia-reperfusion and traumatic injury.
What cell-death pathways are modulated in experiments testing this therapy?
Research indicates reductions in apoptotic signaling (caspase activation, Bax/Bcl-2 ratio), altered autophagy markers via AMPK/mTOR pathways, and suppression of inflammasome-driven pyroptosis such as NLRP3–caspase-1. Modulating these routes can improve neuronal survival after injury.
How robust is the evidence from animal models for functional recovery after nerve injury?
Many rodent studies show positive effects on tissue preservation, reduced oxidative damage, and better behavioral outcomes. However, heterogeneity in models, dosing, and endpoints means results are promising but not yet conclusive for human therapy without further translational work.
Which molecular pathways are most often cited when explaining observed effects?
Nrf2/HO-1 activation appears frequently as an antioxidant defense mechanism. NF-κB suppression links to reduced inflammatory gene expression, and MAPK family members (ERK, p38, JNK) are used to explain stress-response modulation. Studies combine pathway readouts with functional data to suggest mechanisms.
Do studies show benefits for neuropathic pain following partial nerve injury?
In mouse models of partial sciatic nerve ligation, reduced mechanical allodynia and thermal hyperalgesia have been reported alongside lower oxidative stress markers in spinal cord and dorsal root ganglia. Timing and dosing influence whether effects appear during induction or maintenance phases of pain.
Can findings from wound healing research inform nerve repair expectations?
Yes. Improved re-epithelialization, extracellular matrix remodeling, and enhanced vascularization observed in some wound studies suggest a more regenerative microenvironment. Those processes can indirectly support nerve-supportive conditions, though direct translation requires caution.
What are the main limitations when interpreting preclinical claims for human use?
Key constraints include differences between animal models and human pathology, variability in dosing regimens, limited long-term outcome data, and inconsistent endpoints across studies. These factors complicate direct translation to clinical recommendations.
How should consumers view wellness products that deliver dissolved gas in sealed containers?
Sealed storage preserves dissolved levels for a limited time; concentration and timing matter. Bottled solutions may provide low, chronic exposure suitable for general wellness claims but do not replicate acute dosing used in many lab models. Safety profiles in human trials remain limited, so consumers should seek reputable providers and clinical guidance.
Is there any safety concern reported in preclinical research?
Animal studies report a favorable safety profile with no formation of known toxic metabolites and selective antioxidant action. Still, clinical safety data are incomplete, and proper medical oversight is recommended for therapeutic use, especially in acute medical settings.
Where can interested readers learn more locally about services and schedules at Wellness Concept Malaysia?
Wellness Concept Malaysia lists regular hours for in-person visits: Monday through Friday 9:30 am–6:30 pm, Saturday 10:00 am–5:00 pm, and closed on Sunday. Visitors should confirm availability and any booking requirements before attending.


