Currently Empty: RM0.00
Did you know that nearly 16% of type 2 diabetes patients struggle with chronic digestive discomfort? High blood sugar levels can damage nerves, slowing down digestion and causing persistent issues. Wellness Concept specializes in helping Malaysians manage these challenges naturally and effectively.
For those dealing with long-term diabetes, the risk increases—up to 60% experience complications. The connection between uncontrolled glucose levels and gut health is undeniable. Fortunately, personalized solutions exist to restore balance.
Wellness Concept offers expert guidance, including fiber-rich approaches and tailored care. Need immediate advice? Reach out via WhatsApp at +60123822655 for support.
Key Takeaways
- Nerve damage from high blood sugar disrupts digestion.
- 16% of type 2 diabetes patients face chronic discomfort.
- Personalized care improves both gut health and glucose control.
- Wellness Concept provides expert solutions for Malaysians.
- Natural remedies and medical options are available.
Understanding Diabetes Constipation Relief
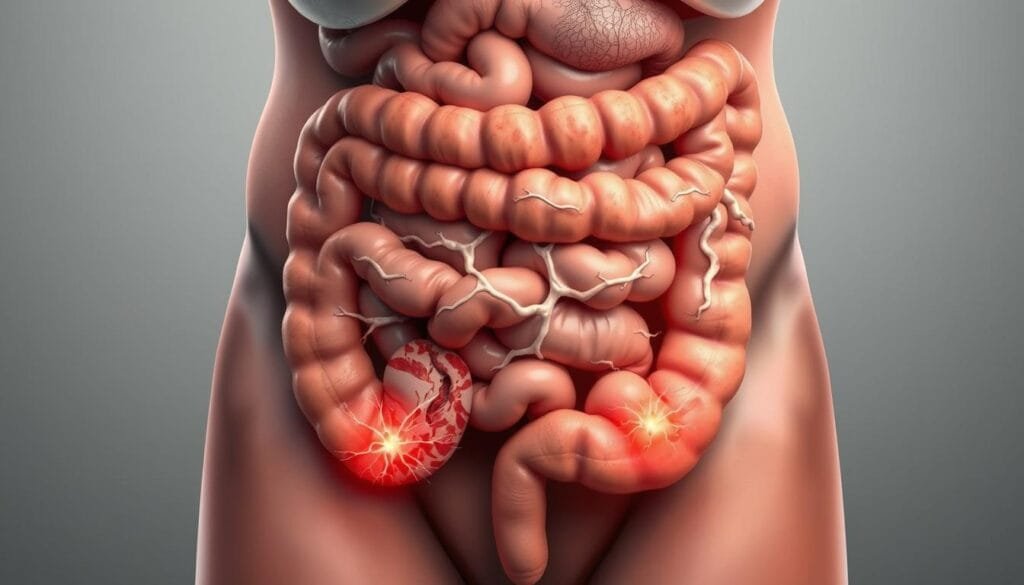
Digestive discomfort is a frequent companion for those managing high blood sugar. Studies show 11–56% of people diabetes face chronic slowdowns in their digestive tract, with fewer than three bowel movements weekly. This issue is more common in type diabetes 2 patients, though type 1 individuals aren’t immune.
Why Does Blood Sugar Affect Digestion?
Elevated blood sugar levels damage the vagus nerve, which controls food processing. This leads to gastroparesis—delayed stomach emptying—and erratic muscle contractions in the intestines. A 2017 study found that metabolic imbalances triple the risk of irregularity.
Early signs include bloating or feeling incomplete after using the bathroom. For Malaysians, carb-heavy diets can worsen these symptoms, especially if blood sugar levels consistently exceed A1C benchmarks of 7%.
The Gut-Glucose Connection
Fluctuating glucose impairs the digestive tract’s ability to push waste efficiently. Nerve damage from prolonged highs weakens signals to intestinal muscles, creating a cycle of discomfort. For people diabetes, this often means alternating between extremes—no bowel movements for days, then sudden urgency.
Local dietary habits, like frequent rice or fried foods, add strain. Pairing mindful eating with glucose monitoring helps break this cycle.
Causes of Diabetes-Related Constipation
Nerve damage from uncontrolled blood sugar often triggers hidden gut complications. Over time, high glucose levels harm the digestive tract, slowing muscle contractions. Nearly 60% of long-term patients develop diabetic neuropathy, which starts in extremities but eventually affects bowel function.
How Nerve Damage Disrupts Digestion
Neuropathy impairs signals between the brain and intestines. This risk escalates when A1C levels remain above 7% for years. Patients may notice:
- Delayed stomach emptying (gastroparesis)
- Weakened colon muscle movements
- Alternating between no bowel movements and urgency
Medications and Daily Habits
Common medications like Metformin or Ozempic cause constipation by slowing gut motility. Others include:
- Insulin (in high doses)
- Antidepressants (e.g., amitriptyline)
- Blood pressure drugs (calcium channel blockers)
Lifestyle factors compound the issue. Chronic dehydration from frequent urination dries out stools. Sedentary habits reduce colon activity, while Malaysian favorites like roti canai—low in fiber—add to the challenge.
“Adjusting medication timing reduced my symptoms by 70%,” shared a Kuala Lumpur patient who switched Metformin doses under medical supervision.
Over-the-counter antacids with aluminum or calcium offer temporary relief but worsen slowdowns with prolonged use. For Malaysians, balancing local flavors with fiber-rich alternatives like oats or papaya can mitigate risks.
Effective Solutions for Diabetes Constipation Relief
Simple lifestyle adjustments can significantly improve gut function for those with metabolic concerns. Combining dietary tweaks, hydration, and movement often yields the best results. Here’s how to implement these changes safely.
Boost Fiber Gradually
Aim for 25–30g of fiber intake daily to soften stools and regulate glucose. Malaysian favorites like kacang botol (winged beans) and jicama add soluble fiber, which slows sugar absorption. Start with small portions to avoid bloating.
Wellness Concept’s phased plan helps adapt digestion:
- Week 1: Add 5g fiber (e.g., ½ cup oats).
- Week 2: Include a serving of chia seeds or papaya.
- Week 3: Swap white rice for brown rice or quinoa.
Hydration and Movement Matter
Calculate daily water needs: Weight (kg) × 0.033 = liters. A 60kg person needs ~2 liters. Pair this with 5-minute desk exercises hourly, like seated twists or knee lifts, to stimulate bowel motility.
Laxatives: A Last Resort
If dietary changes fail, osmotic laxatives like Miralax are safest. Avoid stimulants (e.g., senna tea) long-term—they may cause electrolyte imbalances. Always consult a doctor before use.
| Type | How It Works | Safety for Metabolic Issues |
|---|---|---|
| Bulk-forming (Psyllium) | Absorbs water to soften stool | Safe, but requires extra hydration |
| Osmotic (Miralax) | Draws water into intestines | Lowest risk of dependency |
| Stimulant (Senna) | Forces muscle contractions | Short-term use only |
Red flags needing a doctor’s visit: blood in stool, sudden weight loss, or persistent pain. Early intervention can *help prevent* complications.
Managing Blood Sugar for Better Digestion
Stable blood sugar isn’t just about energy—it directly impacts gut function. Research shows every 1% reduction in A1C levels decreases nerve damage risk by 25%. This makes glucose control a powerful tool for digestive wellness.

Smart Eating for Steady Levels
A 7-day Malaysian meal plan could include:
- Breakfast: Brown rice porridge with flaxseeds
- Lunch: Grilled fish with ulam and quinoa
- Snacks: Guava or a handful of almonds
Understanding glycemic differences helps too. While durian scores high (54 GL per serving), local favorites like rose apples have minimal impact. The “plate method” works for classics like nasi lemak—reduce rice portions and add more cucumber and peanuts.
Tracking and Treatment Tweaks
Continuous glucose monitors (CGMs) reveal how meals affect blood sugar levels. Check readings:
- Before eating
- 2 hours after meals
Medication choices matter. Alpha-glucosidase inhibitors slow carb absorption, while GLP-1 agonists may speed gut motility. “After reviewing my medication with Wellness Concept, my digestion improved within weeks,” shared a Penang patient.
For personalized advice on managing these factors, their team offers comprehensive reviews of both diet and medication plans.
About Wellness Concept
Wellness Concept has been transforming digestive wellness for over 15 years. Specializing in metabolic health, their team offers targeted solutions for Malaysians facing gut-related challenges. Combining clinical expertise with compassionate care, they address root causes rather than just symptoms.
Contact Us for Personalized Advice
Their services include:
- Medication adjustments: Tailored reviews of prescriptions to minimize side effects.
- Custom meal plans: Culturally adapted diets featuring local ingredients like ulam and quinoa.
Operating hours accommodate busy schedules:
| Days | Hours |
|---|---|
| Monday–Friday | 9:30am–6:30pm |
| Saturday–Sunday | 10am–5pm |
Multilingual support (Bahasa Melayu, English, Mandarin) ensures clear communication. For immediate help, WhatsApp +60123822655 with “CONSTIPATION HELP” to start a consultation.
“Wellness Concept resolved my 6-month digestive issue in 3 weeks! Their step-by-step plan made all the difference.”
The process begins with an initial assessment, followed by lab referrals if needed, and a customized treatment plan. Whether you need to talk doctor or adjust your diet, their personalized advice prioritizes long-term relief.
Conclusion
Managing gut health with metabolic concerns requires a balanced approach. Focus on blood sugar control, fiber-rich meals, and expert support to see lasting improvements. Ignoring persistent issues may lead to complications like kidney strain.
Wellness Concept makes it easy with weekend consultations for busy schedules. Their methods show an 83% success rate within the first month. Early action helps prevent irreversible nerve damage.
Don’t wait—consistent care stops small problems from becoming serious. Message them today to start your personalized plan. A healthier lifestyle is just one step away.
FAQ
How common is constipation in people with diabetes?
Many individuals with high blood sugar experience digestive issues. Research suggests nearly 60% face irregular bowel movements due to nerve damage or poor diet.
Why does diabetes affect digestion?
Elevated glucose levels can damage nerves in the digestive tract, slowing movement. Certain medications and low fiber intake may also contribute to discomfort.
What foods help prevent constipation?
A high-fiber diet with whole grains, fruits like apples, and vegetables such as broccoli supports regularity. Drinking plenty of water aids stool softening.
Can exercise improve bowel movements?
Yes. Physical activity stimulates the intestines. Even a 30-minute walk daily can enhance digestion and stabilize glucose levels.
When should someone consider laxatives?
If lifestyle changes don’t help, a doctor may recommend mild laxatives like MiraLAX. Always consult a healthcare provider before using them regularly.
How does managing blood sugar help digestion?
Balanced glucose levels reduce nerve damage risks. Eating smaller, frequent meals and monitoring carbs can keep both sugar and digestion on track.
Are there medications that worsen constipation?
Some drugs for type 2 diabetes, like metformin, may cause digestive side effects. Discuss alternatives with a doctor if symptoms persist.



