Currently Empty: RM0.00
Surprising fact: about 65% of people worldwide have reduced ability to digest milk sugar after childhood — and many only notice symptoms later in life.
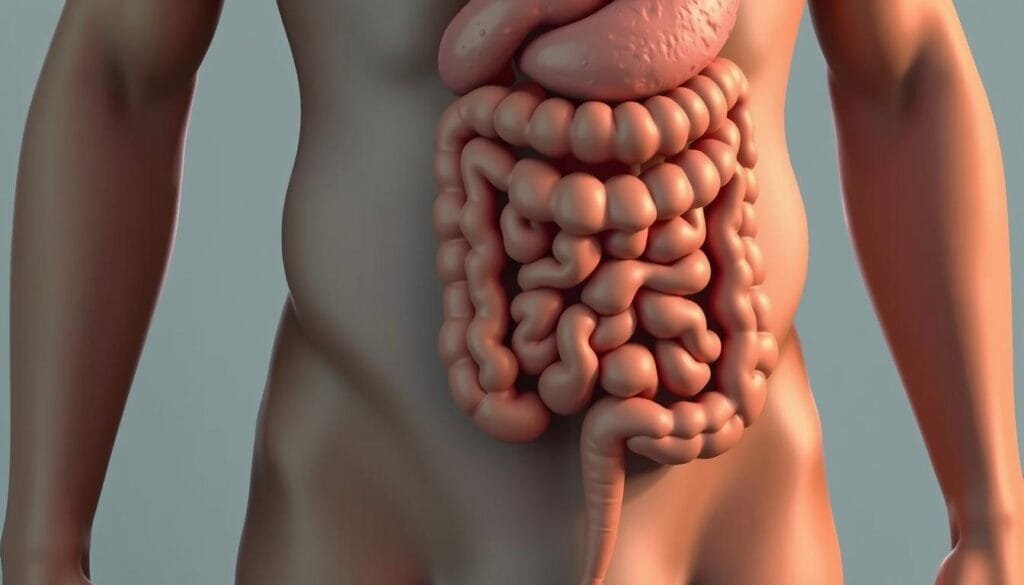
This guide looks at why low lactase activity sends undigested milk sugar to the colon, where bacteria ferment it and cause gas, bloating, cramps, or diarrhea. Symptoms usually show up 30 minutes to two hours after eating dairy.
Experts say options include low‑milk strategies, lactase enzyme tablets or drops, and choosing fermented dairy like yogurt with live cultures, which many people tolerate better than milk.
Practical note: live cultures are generally safe and might ease digestion for some, but they are not a cure. For friendly product guidance in Malaysia, contact Wellness Concept on WhatsApp at +60123822655. Business hours: Monday–Friday 9:30 am–6:30 pm; Saturday 10 am–5 pm; Sunday Closed.
Key Takeaways
- Lactase deficiency leaves milk sugar to ferment, causing common digestive symptoms.
- Symptoms tend to appear within 30 minutes to two hours after dairy.
- Fermented dairy with live cultures is often easier to handle than plain milk.
- Live cultures may help some people but do not cure the condition.
- Hydrogen breath testing can confirm the diagnosis and guide care.
- Contact Wellness Concept on WhatsApp for local product advice and support.
At a glance: lactose intolerance and whether probiotics can help
Many people notice tummy upset after dairy, and quick clues help point to low milk‑sugar digestion.
Quick takeaway for readers in Malaysia
- What to expect: symptoms often start 30–120 minutes after milk or other lactose‑containing foods and commonly include gas, bloating, cramps, or loose stools.
- Food choices: small servings, hard cheeses, lactose‑free products, and yogurt with active cultures are often better tolerated than plain milk.
- Testing: a hydrogen breath test can confirm the problem by showing elevated breath hydrogen after a lactose challenge.
How probiotics fit into a broader management plan
Probiotics are generally safe and may also help reduce gas and discomfort when used with low‑lactose strategies and lactase enzyme products.
They are one tool among practical steps: adjust serving sizes, pair milk with meals, try fermented dairy, and consider a short trial while tracking changes.
Tip: Malaysians seeking product recommendations can WhatsApp Wellness Concept at +60123822655. Hours: Mon–Fri 9:30 am–6:30 pm; Sat 10 am–5 pm; Sun Closed.
| Action | Why it helps | When to try | Notes |
|---|---|---|---|
| Smaller servings | Reduces undigested sugar reaching the colon | Immediately | Pair with meals to slow digestion |
| Yogurt with live cultures | Supports lactose breakdown | Daily trial for 2–4 weeks | Often easier than milk |
| Lactase enzyme products | Replaces missing enzyme activity | Before dairy intake | Use as directed |
| Hydrogen breath test | Confirms diagnosis | When certainty is needed | Ask a healthcare provider |
Understanding lactose intolerance: causes, symptoms, and timing
If the gut cannot split milk sugar, that sugar reaches the colon and resident microbes ferment it, producing gas and acids that irritate the bowel.
Why the body struggles to digest milk sugar
The small intestine must make enough lactase, the enzyme that splits lactose into absorbable sugars. When lactase drops, the sugar cannot cross the intestinal wall efficiently.
Undigested sugar then reaches the colon, where bacteria convert it to gases and short‑chain fatty acids. That process explains the common discomfort after dairy products.
Common symptoms and typical timing
Typical symptoms include gas, bloating, cramps, and diarrhea. These signs often start within 30 minutes to two hours after eating or drinking dairy.
People can track which foods and portion sizes trigger trouble to find a personal threshold. Because other gut conditions can cause similar signs, testing helps confirm the cause.
Types of this condition
- Primary — age‑related decline in lactase; most common.
- Secondary — follows intestinal injury (eg, gastroenteritis, inflammatory bowel disease); may improve as the lining heals.
- Developmental — seen in premature infants and often resolves with maturation.
- Congenital — rare genetic absence of lactase from birth.
If symptoms persist or are severe, Malaysians can contact Wellness Concept on WhatsApp at +60123822655 for product guidance and ask their clinic about testing; hours: Mon–Fri 9:30 am–6:30 pm, Sat 10 am–5 pm.
| Issue | Cause | Typical time to symptoms |
|---|---|---|
| Primary deficiency | Age‑related lower lactase production | 30–120 minutes |
| Secondary deficiency | Injury to small‑intestine lining | Variable; depends on exposure |
| Developmental | Immature gut in preterm infants | Immediate in affected newborns |
| Congenital | Genetic absence of enzyme | From birth |
Learn more about practical options and products at this guide.
How probiotics may support lactose digestion in the gut
Some helpful strains make an enzyme that mimics lactase and eases milk sugar digestion in the small intestine.
How microbial enzymes help
Certain beneficial bacteria produce beta‑galactosidase, an enzyme that can break lactose into simpler sugars. This added enzymatic activity helps when the body’s own lactase is low.
The result is less undigested milk sugar reaching the colon and fewer gas and bloating episodes. These effects reduce symptoms without altering the small intestine’s long‑term enzyme production.
Why fermented dairy often feels gentler than milk
Fermented dairy products such as yogurt slow gastric emptying, giving more time in the small intestine to digest lactose. Live cultures deliver on‑site enzymatic help, so the same lactose content in milk may be harder to tolerate than in yogurt or similar dairy products.
- Certain bacteria supply beta‑galactosidase to break lactose into absorbable sugars.
- Enzymatic support in the gut helps when native lactase levels are low and improves digestion.
- Delayed stomach emptying in fermented foods increases contact time for lactose processing.
Practical note: For help choosing probiotics or yogurts with live cultures available in Malaysia, message Wellness Concept at +60123822655 during business hours.
What the evidence says: probiotics and lactose intolerance symptoms
Clinical trials have tested specific strains to see whether targeted microbes ease common dairy-related discomfort.
Key strains studied
Lactobacillus acidophilus has been the focus of several trials. DDS‑1 (10 billion CFU) showed meaningful drops in diarrhea and cramps versus placebo.
L. acidophilus NCFM and Bifidobacterium lactis BB‑12 also improved dairy tolerance during supplementation. These strains add enzymatic support that helps break lactose in the gut.
Clinical findings
Randomized studies and reviews report fewer episodes of gas, bloating, and loose stools in many participants. Overall symptom scores often improved while people took the products or ate yogurt with active cultures.
Limits of the evidence
Important: improvements target symptom relief, not a cure. Benefits tend to be greater for those with mild to moderate maldigestion who still want some dairy.
- Key trials: DDS‑1 reduced diarrhea and abdominal pain in crossover studies.
- Other strains: NCFM and BB‑12 improved tolerance during use.
- Realistic goal: symptom reduction and added dietary flexibility, not restored enzyme production.
Malaysians seeking guidance on clinically studied strains can WhatsApp Wellness Concept at +60123822655. Hours: Mon–Fri 9:30 am–6:30 pm; Sat 10 am–5 pm.
Probiotics for lactose intolerance: do they work?
A practical, time‑limited test gives clear feedback on whether a chosen supplement adds meaningful relief while keeping some milk in the diet.
When a trial may be worth trying and how long to test
They may also help some people who still want dairy in small amounts. A sensible protocol is a daily dose for 2–4 weeks, taken at a consistent time, while logging meals and symptoms.
Most trials evaluate effects over several weeks, so short trials can miss benefits. Track portion size, meal timing, and any changes to symptoms to judge results.
Combining supplements with low‑lactose strategies
Combine approaches for better results: use lactose‑free products, try lactase enzyme tablets or drops, and eat milk with meals to slow digestion.
- Start with strains supported by evidence and monitor tolerance.
- Expect improved tolerance and comfort rather than a cure of the enzyme shortage.
- If symptoms persist or worsen, pause the trial and consult a healthcare professional.
For quick guidance on a 2–4 week trial protocol and product options in Malaysia, WhatsApp Wellness Concept at +60123822655 during business hours.
How to use probiotics safely and effectively
Begin with small amounts and a clear log—this simple routine shows whether a chosen supplement and food choices improve digestion.

Step-by-step: start low, monitor, adjust with meals
Start low and go slow. Take a modest daily dose at the same time each day and keep a short diary of meals and symptoms for two weeks.
Try taking the product with your largest dairy-containing meal to give enzymes and microbes the best chance to help.
Choosing products: strains, CFU, yogurt and supplements
Pick products that list specific strains and clear CFU counts. Yogurt with active cultures can be a practical first choice.
Look for supplements that cite strains studied for milk tolerance and stay within recommended dosing.
Diet tips from experts: lactose-free options and bone health
Use lactose-free milk or smaller servings of regular milk (up to 4 oz) and prefer hard cheeses with less sugar.
Consider lactase tablets or drops added to milk as a layered strategy alongside microbial support.
Protect bone health by getting calcium from leafy greens, fortified juices, canned fish, and vitamin D from diet or supplements.
Who should consult a healthcare professional first
Those who are immunocompromised, acutely ill, or managing complex GI conditions should speak to a healthcare professional before starting new products or supplements.
Need help selecting strains or lactose‑free options available locally? Contact Wellness Concept on WhatsApp at +60123822655. Hours: Mon–Fri 9:30 am–6:30 pm; Sat 10 am–5 pm; Sun Closed.
Local guidance and support in Malaysia
Getting professional input quickly clarifies whether symptoms come from milk sugars or another gut condition. A healthcare provider can arrange objective testing and suggest a tailored plan that fits daily life.
Talk to a healthcare provider about testing
A hydrogen breath test confirms maldigestion by measuring breath hydrogen after a milk challenge. This helps clinicians tell apart milk-related reactions and conditions such as irritable bowel syndrome.
When a chronic disease or damage to the gut lining is suspected, coordinated care across the digestive system gives the best outcomes.
Contact Wellness Concept for local product guidance
Malaysians can message Wellness Concept on WhatsApp at +60123822655 for friendly advice on available products and strains. The team helps match choices to budget and preference.
- Speak with a healthcare provider to discuss the hydrogen breath test and a tailored plan.
- If symptoms overlap with irritable bowel or bowel syndrome, clinicians will suggest next steps.
- People wanting local product options can WhatsApp Wellness Concept for real-time suggestions on products and probiotics.
- Business hours: Mon–Fri 9:30 am–6:30 pm; Sat 10 am–5 pm; Sun Closed.
Conclusion
A practical next step is a short, structured trial that pairs known strains such as Lactobacillus acidophilus (DDS‑1, NCFM) and Bifidobacterium lactis (BB‑12) with small servings, yogurt with active cultures, or a lactase enzyme. Evidence shows these measures can reduce symptoms like gas and bloating for some people with lactose intolerance.
These approaches ease the gut during dairy exposure but do not restore long‑term lactase production. If symptoms persist, a hydrogen breath test and a visit to a healthcare professional help confirm diagnosis and guide choices.
Malaysians seeking product suggestions can WhatsApp Wellness Concept at +60123822655 (Mon–Fri 9:30 am–6:30 pm; Sat 10 am–5 pm; Sun Closed) for friendly, local guidance.
FAQ
What causes someone to have trouble digesting dairy?
Trouble digesting milk and other dairy products happens when the small intestine makes too little lactase, the enzyme that breaks down milk sugar. Without enough lactase, lactose reaches the colon undigested, where bacteria ferment it and trigger symptoms such as gas, bloating, cramps, and diarrhea.
Can live culture yogurt be easier to tolerate than regular milk?
Yes. Yogurt with active cultures contains bacteria that produce beta‑galactosidase, a lactase‑like enzyme. Those microbes begin breaking down milk sugar during fermentation and continue to help in the gut, so many people find yogurt causes fewer symptoms than plain milk.
Are supplements that contain beneficial bacteria helpful for symptom relief?
Some supplements containing specific strains have shown modest symptom improvement in trials, especially for gas and bloating. They are not a cure, but they may reduce discomfort for people with mild to moderate enzyme deficiency when used alongside dietary changes.
Which bacterial strains have the strongest research supporting benefit?
Strains most often studied include Lactobacillus acidophilus (examples: DDS‑1, NCFM) and Bifidobacterium lactis (BB‑12). These strains have been linked to improved lactose digestion and lower symptom scores in some clinical trials.
How long should someone try a supplement to know if it helps?
A practical trial lasts about two to four weeks. That gives time for the gut to respond and for the person to track changes in gas, bloating, and stool. If there’s no clear benefit after a month, stopping the product is reasonable.
Should people use a drop‑in lactase enzyme instead of beneficial bacteria?
Lactase enzyme drops or tablets work differently: they replace the missing enzyme and can give faster, more predictable relief when taken with dairy. Beneficial bacteria may reduce symptoms over time but usually act less immediately than lactase supplements.
Are there safety concerns or side effects to consider?
Most people tolerate these products well, but mild bloating or gas can occur at the start. People with serious immune problems or critical illness should check with a healthcare professional before taking live microbial supplements.
Can combining a supplement with low‑lactose eating improve results?
Yes. Pairing a microbial product or lactase enzyme with reduced‑lactose choices, such as lactose‑free milk, fermented dairy, or small portions of dairy, often gives the best symptom control while maintaining calcium and vitamin D intake.
How should someone choose a product to try?
Look for strains backed by clinical research, a clear CFU count at the end of shelf life, and storage instructions. Fermented foods like yogurt with active cultures are cost‑effective options. For supplements, prefer reputable brands and check labels for strain names.
Who should get tested before trying supplements or changing diet?
People with frequent or severe symptoms, sudden onset of intolerance, unintentional weight loss, blood in stool, or a history of inflammatory bowel disease should see a healthcare provider. A hydrogen breath test can confirm reduced lactase activity and guide treatment.
Where can someone in Malaysia get local support or testing?
They should speak with a local healthcare provider for testing such as the hydrogen breath test and personalized advice. For product guidance, contact Wellness Concept on WhatsApp at +60123822655 during business hours: Mon–Fri 9:30 am–6:30 pm, Sat 10 am–5 pm.



