Currently Empty: RM0.00
Surprising fact: recent research notes measurable increases in intestinal permeability in many people, yet “leaky gut” is not a formal diagnosis.
Wellness Concept offers a practical, science-aligned path to better gut health for people in Malaysia. The plan explains how the intestinal barrier normally protects the body and what happens when its integrity is stressed by diet, stress, alcohol, or certain drugs.
The guide sets clear expectations about timelines and outcomes. It shows how targeted probiotics, balanced foods, stress reduction, and sleep habits can support barrier function and reduce inflammation and common symptoms over a 4–8 week roadmap.
Readers can contact Wellness Concept on WhatsApp at +60123822655 during business hours: Monday–Friday 9:30 am–6:30 pm, Saturday 10 am–5 pm. This friendly support helps adapt plans to local routines and food choices.
Key Takeaways
- Increased intestinal permeability is measurable; “leaky gut” is not a formal diagnosis.
- A combined approach—probiotics, diet, sleep, and stress control—supports barrier integrity.
- Expect gradual improvement; a 4–8 week roadmap helps track comfort and tolerance.
- Wellness Concept offers WhatsApp guidance at +60123822655 during Malaysian business hours.
- Consult a clinician first if severe symptoms appear; use evidence-aligned guidance for safety.
Understanding intestinal permeability and the gut barrier
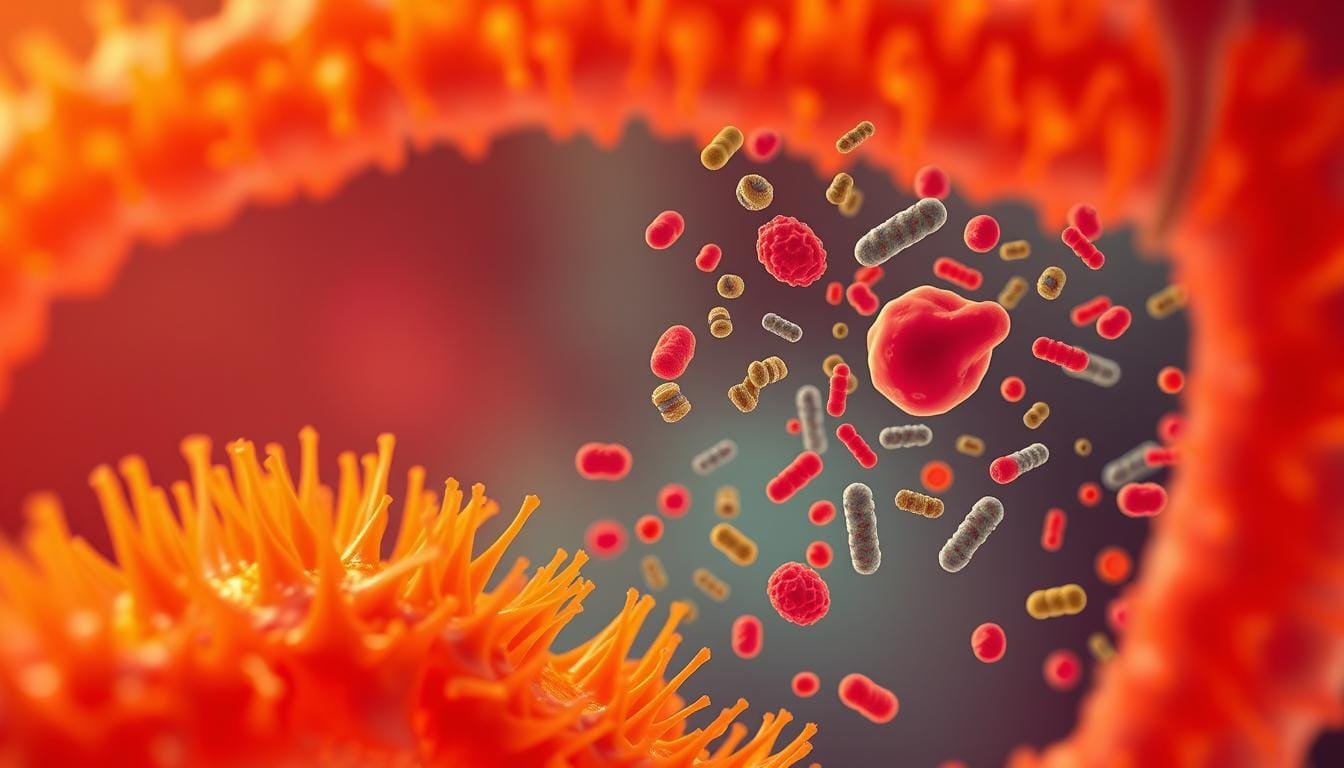
Multiple defenses in the gut act together to let nutrients through while keeping threats out. This layered system balances absorption and protection so the body gets what it needs without undue exposure to microbes or toxins.
Layers of defense: microbiota, mucus, epithelial cells, and immune components
The microbiota layer competes with pathogens and creates metabolites that support barrier function. Friendly bacteria help maintain balance and back up the immune system along the intestinal tract.
The mucus and chemical layer vary by region: thin in the small intestine, dual-layered in the colon. Mucins like MUC2, secretory IgA, and antimicrobial peptides reduce direct contact between microbes and epithelial cells.
The epithelial layer is a single sheet of rapidly renewing cells joined by tight junctions. Proteins such as occludin, claudins, JAMs, and ZO-1/2/3 act as adjustable gates to control paracellular permeability.
- Tight junctions respond to signals via MLCK, MAPK, PKC/PKA/PKG pathways.
- Beneath the epithelium, T cells, B cells, macrophages, and dendritic cells monitor luminal content.
- When signaling is altered, studies link loosening of junctions to increased intestinal permeability and low-grade inflammation.
Why this matters: appreciating the many cells and immune components explains why increased permeability appears in several conditions and why targeted nutrition and supportive strategies often work best.
What leaky gut means in research today
Modern studies separate measurable changes in the intestinal barrier from popular labels that lack clinical consensus.
Recognized features versus unproven diagnoses
Research shows that increased intestinal permeability appears in some bowel disease such as inflammatory bowel disease and celiac disease. In those settings, higher permeability often co-occurs with inflammation and is treated as a feature, not the sole cause of disease.
Some studies detect microbial products or fragments in the bloodstream in GI and liver conditions. These findings suggest possible links to broader symptoms, but causes are usually multifactorial and not explained by permeability alone.
“Permeability changes are a piece of the puzzle — not a standalone diagnosis.”
- Measured change vs. syndrome: leaky gut is used casually but is not a formal medical diagnosis.
- Clinical context matters: symptoms like bloating are common and nonspecific.
- Ongoing research: investigators test whether permeability shifts can precede some conditions, but evidence is limited.
| Finding | What it suggests | Clinical note |
|---|---|---|
| Increased permeability | Seen in IBD and celiac | Often a feature of inflammation |
| Bacterial products in blood | Possible systemic effects | Contributors often include liver or immune changes |
| Sporadic symptom overlap | Bloating, discomfort | Requires careful evaluation |
Conditions associated with increased intestinal permeability
Several conditions show clear links to increased intestinal permeability. Studies often report measurable changes in the barrier in specific inflammatory disorders.
Inflammatory bowel disease — including Crohn’s disease and ulcerative colitis — is most consistently associated with shifts in permeability. Celiac disease also shows barrier changes that occur alongside immune reactions to gluten.
Irritable bowel syndrome and certain liver-related conditions, such as alcoholic and nonalcoholic fatty liver disease, have been linked to altered intestinal permeability. Researchers have also discussed connections to metabolic conditions like obesity and diabetes, though permeability usually appears as a contributory feature rather than the sole cause.
“In many cases, chronic inflammation and immune activation precede or accompany permeability shifts.”
- Permeability changes appear across bowel disease types and in celiac disease.
- Some liver and metabolic conditions show associations, but causation is not established.
- Recognizing these links helps clinicians suggest supportive strategies such as targeted nutrition, stress management, and evidence-aligned probiotic use as adjuncts.
Common symptoms linked to barrier dysfunction
Everyday symptoms like bloating and irregular stools can hint at subtle changes in intestinal barrier performance.
People often report abdominal pain, bloating, indigestion, or altered bowel habits when they suspect barrier issues. These complaints are common and nonspecific, so they do not confirm increased permeability or leaky gut on their own.
Some patients notice fluctuating food tolerance or new sensitivities. These shifts may reflect changes in bacteria balance, motility, or low-grade inflammation rather than permeability alone.
Extra-digestive effects such as fatigue or skin irritation can occur alongside digestive symptoms, but they are not reliable markers by themselves.
- Keep a simple symptom log: note meals, stress, sleep, and timing of effects to spot triggers.
- Track patterns: this helps guide diet, lifestyle, and targeted interventions.
- Seek care: persistent or worsening signs should prompt medical evaluation to rule out specific bowel disease.
For readers in Malaysia interested in strategies to ease bloating and related complaints, see the guide on probiotics for gas, bloating and constipation for practical steps and support.
How probiotics can support tight junctions and barrier function
Certain probiotic strains act on cellular pathways to strengthen barrier links between intestinal cells. These actions help maintain selective permeability and support overall barrier function.
Strain-specific actions: reinforcing tight junctions, mucus, and SCFA production
Lactobacillus plantarum has been shown in some studies to boost expression of proteins that form tight junctions. That helps epithelial cells hold together under stress.
Bifidobacterium lactis contributes to short-chain fatty acid production such as butyrate, which fuels colon cells and supports barrier function.
Saccharomyces boulardii can increase mucus thickness, complementing the epithelial layer and reducing local inflammation.
Synergy: why multispecies blends may outperform single strains
Combining strains often yields complementary effects: tighter junction control, more SCFA, and stronger mucus. This cooperative mix can speed rebalancing of gut bacteria and ease inflammation.
- Modulation of cytokines and mucin production supports epithelial integrity.
- Targeted blends pair actions—tight junction support, SCFA boost, and mucus reinforcement—for clearer outcomes.
Takeaway: a tailored, multispecies plan used alongside diet and lifestyle offers the best chance to improve permeability and long-term function.
Repair your gut lining with probiotic: a practical, step-by-step plan
A practical timetable shows how steady dosing and gentle diet steps can shape early responses to a multispecies regimen. The goal is gradual support of barrier integrity while tracking tolerance and comfort.
Week-by-week roadmap for 4–8 weeks
Week 1–2: Start a multispecies probiotics at the label dose with meals. Drink enough water and favor gentle, fiber-rich foods to reduce abrupt changes.
Week 3–4: Keep dosing steady. Add prebiotic foods slowly (oats, bananas, asparagus). Try small portions of fermented items if they are well tolerated.
Week 5–6: Reassess timing and dose based on digestive comfort. Add stress-reduction steps and steady sleep to help gut–brain balance and recovery.
Week 7–8: Review trends in bloating, stool consistency, energy, and food tolerance. Adjust the plan and consult a clinician if needed.
Tracking changes: digestive comfort, energy, and food tolerance
Daily notes on meals, symptoms, sleep, and stress help identify triggers and responses. This record guides safer choices and supports long-term function and integrity of the lining.
- What to track: bloating frequency, stool form, energy, and new intolerances.
- Pairing tips: include nutrient-rich, anti-inflammatory foods to support epithelial repair and microbial balance.
- Safety: if major symptoms persist or worsen, pause the plan and seek medical advice.
| Week | Focus | Key actions |
|---|---|---|
| 1–2 | Introduce | Start probiotics; hydrate; gentle fiber |
| 3–4 | Build | Add prebiotics slowly; fermented foods as tolerated |
| 5–6 | Refine | Adjust timing/dose; add stress and sleep habits |
| 7–8 | Evaluate | Review symptoms; consult professional if needed |
Selecting evidence-informed probiotic strains for barrier integrity
Not all live cultures act the same; selection matters when targeting barrier health. Choosing strains based on documented actions helps align supplements with goals for permeability and inflammation control.
Lactobacillus, Bifidobacterium, and beneficial yeast considerations
Lactobacillus plantarum is noted in several studies for supporting tight junctions and cell signaling. Bifidobacterium lactis aids short-chain fatty acid production that fuels colon cells and supports integrity.
Saccharomyces boulardii can thicken mucus and limit pathogen adherence, complementing bacterial actions and reducing local inflammation.
- Choose strains with documented barrier actions (L. plantarum, B. lactis).
- Consider yeast for mucus support and pathogen exclusion.
- Favor multispecies blends that combine complementary mechanisms for broader gut bacteria support.
- Check labels for CFU at end of shelf life, strain names, and storage rules to keep viability.
- Account for needs such as lactose tolerance or FODMAP sensitivity when picking doses and timing.
Practical note: emerging research shows promise, but individual responses vary. They should monitor symptoms, track changes, and pair choices with diet and lifestyle steps that support epithelial cells and long-term function.
Pairing probiotics with prebiotics to boost beneficial bacteria
Combining fermentable foods and live cultures creates an environment where helpful bacteria can grow and produce healing metabolites.
Prebiotics are fermentable fibers that serve as food for microbes. They help beneficial bacteria expand and make short-chain fatty acids (SCFA). SCFA nourish colon cells and support barrier permeability and overall function.
Dietary fibers that fuel microbial balance
Everyday foods such as garlic, onions, bananas, oats, and asparagus supply inulin and FOS. Adding these items slowly can boost microbial activity and enhance effects on digestion over weeks.
- Start low, go slow: small portions limit gas and bloating while building tolerance.
- Meal integration: add prebiotic food to snacks and dishes for steady intake and balanced diet support.
- Pairing benefits: prebiotic fermentation raises SCFA, which may help permeability and gut health when combined with live cultures.
| Food | Fiber type | Likely effect |
|---|---|---|
| Garlic, onions | Inulin, FOS | Feeds bifidobacteria; increases SCFA |
| Bananas, oats | Resistant starch, soluble fiber | Gentle substrate for microbial growth |
| Asparagus | Inulin | Supports mucus and epithelial function |
Tip: this pairing works best as part of a broader plan that includes stress reduction and consistent sleep to support lasting gut function and health.
Integrating probiotic-rich foods into everyday meals
Simple swaps at breakfast and dinner can bring live cultures into everyday meals without extra fuss.
Fermented foods like yogurt, kefir, kimchi, tempeh, miso, and kombucha provide live cultures that boost microbial diversity in the diet. Regular inclusion helps support gut balance and may reduce low-grade inflammation over time.
Yogurt, kefir, kimchi, tempeh, miso, and kombucha: smart ways to include them
- Have a serving of yogurt or kefir at breakfast. Add oats or fruit for fiber and extra nutrients.
- Add kimchi as a tangy side for rice bowls or wraps to introduce varied bacteria and bold flavor.
- Use tempeh in stir-fries or grilled skewers as a fermented plant protein for weekday meals.
- Stir miso into warm (not boiling) broth to keep live cultures and add savory depth.
- Choose kombucha as an occasional swap for sugary drinks; pick lower-sugar varieties.
- Rotate different fermented items to broaden microbial exposure and pair them with a balanced diet.
- Start with small portions to test tolerance and increase slowly as digestion adapts.
| Food | Typical serving | Main benefits | Notes |
|---|---|---|---|
| Yogurt / Kefir | 1 cup | Live cultures, calcium, protein | Pair with oats or fruit |
| Kimchi | 2–3 tbsp | Varied bacteria, flavor boost | Add to rice bowls or sandwiches |
| Tempeh / Miso | 75–100 g / 1 tbsp | Fermented protein, umami nutrients | Cook tempeh; add miso to warm soups |
Anti-inflammatory dietary strategies that support gut lining integrity
Targeted dietary choices help calm inflammation and nourish cells that maintain barrier integrity.
Prioritize whole, minimally processed foods. Plenty of vegetables and quality proteins reduce dietary drivers of inflammation that affect the gut environment.
Emphasize a variety of fiber sources from whole grains, legumes (as tolerated), fruits, and vegetables. This mix feeds diverse microbes and boosts short-chain fatty acid production, which supports barrier integrity.
Choose healthy fats such as olive oil, nuts, seeds, and omega-3-rich fish. Limit refined seed oils and trans fats, which can worsen inflammatory effects and harm long-term health.
- Include polyphenol-rich foods: berries, green tea, turmeric, and colourful produce to add antioxidant support.
- Cut added sugars and ultra-processed snacks to lower glycemic swings and discourage less desirable microbes.
- Consider a time-limited low FODMAP approach under professional guidance for sensitive people to reduce symptom burden while keeping nutrients steady.
Keep meals consistent and enjoyable. A steady eating pattern improves adherence and complements probiotic strategies aimed at improving barrier-related outcomes.
Hydration, sleep, and stress: lifestyle factors that influence permeability
Small, steady habits around hydration and rest help the body maintain cell repair and a balanced microbiome. These daily choices affect microbial communities and the mucus that shields epithelial surfaces.
Stress reduction and sleep hygiene for gut-immune balance
Chronic stress raises cortisol and shifts microbial balance, which can change permeability and how the immune system reacts. Consistent sleep supports nightly cellular repair and healthy epithelial turnover.
“Short, reliable routines often do more for long-term comfort than occasional big changes.”
Practical factors to try:
- Hydration supports the mucus layer that protects epithelial surfaces and keeps the gut resilient.
- Simple 15-minute routines — breathing, light stretch, or meditation — reduce stress levels and calm the gut–brain axis.
- Regular sleep times promote repair, lower cortisol levels, and improve immune response.
- Gentle movement, time outdoors, and social contact lower physiological effects of stress on the body.
| Factor | Main effect | Quick tip |
|---|---|---|
| Hydration | Supports mucus, eases transit | Sip water through the day |
| Sleep | Cell repair, steady immune response | Keep a consistent bedtime |
| Stress | Alters microbes; may raise permeability | Try 15 min daily relaxation |
For a locally tailored approach that pairs simple routines with diet and supplements, see discover a practical probiotic plan for busy lifestyles in Malaysia.
Malaysian-friendly meal ideas for gut health
Using local spices and fermented staples, they can craft meals that feed beneficial bacteria and supply key nutrients.
Local flavours: turmeric curries, tempeh, and fibre-rich sides
Turmeric-rich curries pair well with plenty of vegetables and brown rice. This combo adds fibre and polyphenols that support gut balance and overall health.
- Use tempeh in sambal stir-fries or grilled satay-style skewers as a fermented plant protein that suits local palates.
- Include fibre-rich sides like ulam, lightly pickled vegetables, or seasonal fruit to feed helpful microbes and add texture.
- Add small portions of kimchi or tempeh to noodle bowls or fried rice for an easy probiotic boost within familiar dishes.
- Choose broth-based soups and stir in a bit of miso (avoid boiling) to keep delicate cultures alive and offer soothing effects.
Adjust spice levels to tolerance while keeping diverse ingredients. These dietary ideas make it simple to enjoy familiar food that supports gut resilience and balanced bacteria.
Safety, expectations, and who should seek medical advice
Knowing what to expect and when to seek help makes simple gut-focused plans safer and more effective.
Key point: increased permeability often appears as a feature of broader disease rather than the root cause. Many common symptoms are nonspecific, so changes in comfort do not confirm a diagnosis.
“Barrier findings in studies usually reflect downstream effects of inflammation and other processes.”
Patients should set realistic goals: dietary steps and supplements support the gut environment but do not diagnose or cure underlying disease. Mild digestive effects such as gas or bloating may occur early; these effects often settle with timing or dose adjustments.
- Red flags: unintentional weight loss, blood in stool, fever, persistent vomiting, or severe pain — seek prompt medical attention.
- Complex histories: patients with chronic conditions, on immunosuppressants, or taking multiple medications should consult a clinician before starting new regimens.
- Follow-up: if symptoms persist or worsen, get evaluated to check inflammation levels and other causes.
Practical note: studies show barrier shifts often mirror broader system changes. Personalized assessment helps match care to the clinical picture and keeps patients safe while they try supportive strategies.
When to consult Wellness Concept for a personalized plan
A short consultation can align treatment choices to local food habits and daily routines for better outcomes. Personalized plans often boost adherence and lead to clearer improvements over several weeks.
Business hours and WhatsApp support for Malaysia
WhatsApp: +60123822655.
Business hours: Monday–Friday 9:30 am–6:30 pm; Saturday 10 am–5 pm; Sunday closed. Patients can use WhatsApp for quick guidance or to book an appointment during these times.
What to prepare for your first consultation
- Brief symptom history and any diagnosed medical conditions.
- Current diet notes and usual meal patterns.
- Sleep, stress routines, and recent life factors that may affect health.
- A list of supplements, medications, and prior responses to treatments.
Note: clinicians tailor plans by considering local food, stress, and daily factors to match individual needs. Studies show that tailored advice helps patients track response and manage conditions more safely while supporting long-term health.
Contact Wellness Concept
A short message can make starting a plan easier. For friendly, practical support, patients in Malaysia may contact Wellness Concept by WhatsApp to ask about food choices, targeted supplements, and small stress-management steps that fit daily life.

WhatsApp: +60123822655
Use this number to ask brief questions, book a consult, or get guidance on tracking symptoms and response to a plan. The team helps clarify options so people feel more confident about next steps.
Business hours
Monday 9:30 am–6:30 pm; Tuesday 9:30 am–6:30 pm; Wednesday 9:30 am–6:30 pm; Thursday 9:30 am–6:30 pm; Friday 9:30 am–6:30 pm; Saturday 10 am–5 pm; Sunday Closed.
- Friendly support: quick advice on food swaps and daily routines.
- Patient-focused: practical help to improve adherence and the body’s response.
- Clear guidance: helps patients set realistic steps and track progress.
“Small, consistent steps often yield clearer results than one-off changes.”
Conclusion
Conclusion
Small, steady changes—rather than dramatic fixes—tend to give clearer signals about what improves intestinal barrier function. This balanced view reflects research and studies that place increased permeability in disease contexts rather than as a standalone diagnosis.
Supporting the barrier through targeted probiotics, prebiotic foods, anti-inflammatory meals, good hydration, and stress-aware routines can ease symptoms over weeks. Multispecies supplements plus everyday fermented foods and varied fiber often produce the best effects on microbial balance and function.
Track responses across a 4–8 week window and refine the plan based on results. For personalised advice in Malaysia, contact Wellness Concept on WhatsApp at +60123822655 during business hours for practical guidance.
With patience and consistency, many people see meaningful changes in comfort, energy, and overall gut health.
FAQ
What does increased intestinal permeability mean in research terms?
Increased intestinal permeability refers to weakened barrier function between the gut lumen and the bloodstream. Scientists study features such as altered tight junction proteins, reduced mucus layer, microbial imbalance, and heightened immune activation. These changes can allow larger molecules, microbes, or toxins to cross into circulation and trigger inflammation in some people.
Which layers protect the intestinal barrier?
Several defenses work together: beneficial bacteria that compete with pathogens, a mucus layer that traps microbes, epithelial cells joined by tight junctions, and local immune cells that detect threats. Diet, stress, infection, and medications can affect each layer and overall barrier integrity.
Is "leaky gut" an accepted medical diagnosis?
The term “leaky gut” is popular in media but not a formal medical diagnosis. Researchers acknowledge increased intestinal permeability as a measurable phenomenon linked to certain conditions, while clinical use varies. Careful evaluation is needed to connect permeability changes to symptoms or disease.
Which conditions are associated with higher intestinal permeability?
Increased permeability appears in inflammatory bowel disease, celiac disease, certain infections, and some metabolic and autoimmune conditions. Factors like bacterial overgrowth, chronic stress, and nutrient deficiencies can also contribute to barrier dysfunction.
What symptoms might signal barrier dysfunction?
People may report digestive discomfort, bloating, irregular bowel habits, food intolerances, low energy, or unexplained inflammation. Symptoms are nonspecific, so clinicians consider medical history, labs, and response to interventions when assessing barrier health.
How can probiotics support tight junctions and barrier function?
Certain probiotic strains influence tight junction proteins, enhance mucus production, and produce short-chain fatty acids (SCFAs) that nourish epithelial cells. They also modulate immune responses and compete with pathogenic bacteria, which together can reduce inflammation and support barrier repair.
Do multispecies probiotic blends work better than single strains?
Some evidence suggests multispecies blends offer broader benefits because different strains have distinct mechanisms: immune modulation, SCFA production, or pathogen inhibition. Choice should be evidence-informed and tailored to symptoms and underlying conditions.
Which probiotic strains have research supporting barrier integrity?
Strains from Lactobacillus and Bifidobacterium genera, and certain Saccharomyces boulardii formulations, show promise in studies. Strain-level evidence matters, so consumers should look for clinical trials that tested the specific strains used in products.
How long until someone may notice improvement using probiotics and lifestyle changes?
Changes often appear over weeks. A practical plan usually spans 4–8 weeks to assess effects on digestive comfort, energy, and food tolerance. Tracking symptoms and dietary patterns helps determine whether adjustments or further evaluation are needed.
What role do prebiotics and dietary fiber play?
Prebiotics and fermentable fibers feed beneficial bacteria and boost SCFA production, which supports epithelial health. Foods like oats, legumes, onions, garlic, and resistant starches help sustain a healthier microbial community that can enhance barrier function.
Which fermented foods are easy to add to meals?
Yogurt with live cultures, kefir, kimchi, tempeh, miso, and kombucha are practical options. Small regular servings can introduce diverse microbes and complementary nutrients. People with histamine sensitivity or immune suppression should choose cautiously and consult a clinician.
What dietary strategies reduce inflammation and support the barrier?
An anti-inflammatory approach emphasizes fiber-rich whole foods, omega-3 sources, colorful fruits and vegetables, and limited refined sugars and ultra-processed items. Targeting nutrient adequacy—zinc, vitamin D, and glutamine—also supports epithelial repair.
How do hydration, sleep, and stress affect intestinal permeability?
Dehydration impairs mucosal health, poor sleep dysregulates immune function, and chronic stress increases inflammatory signaling that can alter tight junctions. Stress reduction, consistent sleep, and adequate fluids help maintain barrier integrity and immune balance.
Are there Malaysian-friendly meal ideas that support barrier health?
Local dishes can be adapted: turmeric-rich curries with tempeh or fish, fiber-forward vegetable sides, and sambal-based sauces made with less sugar. Incorporating legumes, whole grains like brown rice, and fermented condiments helps blend culture and gut-supportive nutrition.
Who should seek medical advice before starting probiotics or major diet changes?
People with inflammatory bowel disease, immune suppression, recent surgery, or severe symptoms should consult a healthcare professional. Clinicians can assess diagnostic needs, rule out infections, and recommend evidence-based strains or therapies.
When should someone contact Wellness Concept for a personalized plan?
Individuals seeking tailored guidance on barrier support, strain selection, or dietary plans may contact Wellness Concept. They offer consultations during business hours and can advise on monitoring strategies and safe product choices for Malaysia-based clients.
How can someone reach Wellness Concept for support?
WhatsApp support is available at +60123822655. Business hours are Monday–Friday 9:30 am–6:30 pm and Saturday 10 am–5 pm; closed on Sunday. Clients should prepare recent medical history, current supplements, and a brief symptom diary before the first consultation.