Currently Empty: RM0.00
Surprising fact: in the past decade, shifts in gut microbes were linked to higher obesity and type 2 diabetes risk through gut barrier changes and low‑grade inflammation.
The Ultimate Guide introduces how readers can explore probiotics as a gut‑focused strategy with Wellness Concept. It explains how gut microbiota interact with diet, body composition, and hormones in everyday life in Malaysia.
The article highlights that benefits are strain‑specific and that multi‑strain formulas and synbiotics may enhance outcomes. It previews practical steps: choosing strains, pairing with fibre, and setting a realistic timeline for measurable change.
Contact Wellness Concept via WhatsApp at +60123822655 for tailored selection and dosing support. Business hours: Monday–Friday 9:30 am–6:30 pm; Saturday 10 am–5 pm; Sunday Closed.
Key Takeaways
- Gut microbes can influence insulin and lipid pathways linked to metabolic health.
- Effects are strain‑specific; clinical validation matters.
- Combining selected strains with prebiotic fibres often gives better outcomes.
- Realistic gains include modest weight and visceral fat shifts and improved markers.
- Readers can learn more about targeted lactobacillus options at probiotik lactobacillus.
Understanding Metabolic Syndrome and Why the Gut Matters
To understand risk, one must connect waistline numbers with what happens in the gut. Metabolic syndrome is diagnosed when central obesity pairs with high fasting glucose, raised triglycerides, low HDL, and elevated blood pressure.
- Central obesity drives much of the risk profile and predicts excess visceral fat.
- Fasting glucose, triglycerides, HDL, and blood pressure give a measurable picture of progress.
How the gut ecosystem fuels low-grade inflammation
The gut microbiota communicates with metabolism. It shapes energy harvest, appetite signals, and immune tone.
Dysbiosis can allow bacterial products such as LPS to cross a weakened barrier. This metabolic endotoxemia sparks low-grade inflammation and promotes insulin resistance.
Western-style patterns high in fat and refined carbs — common in urban Malaysian diets — change gut composition. Shifts between Bacteroidetes and Firmicutes often reflect these pressures rather than a single cause.
Even modest improvements in gut ecology can improve insulin dynamics and lipid handling. Restoring barrier function is a key step to reduce chronic inflammation and improve outcomes in metabolic disorders.
Search Intent Decoded: What people in Malaysia want to know about Probiotics for metabolic syndrome
Many Malaysians ask whether targeted gut supplements can shift body fat, blood lipids, and blood sugar in months.
Do they help weight, insulin resistance, and lipids?
Yes, but it depends on the strain and time. A multicenter double-blind randomized controlled trial found Lactobacillus gasseri LG2055 in fermented milk reduced visceral and subcutaneous fat and lowered body weight over 12 weeks.
Other controlled trials link certain Bifidobacterium strains to improved lipid profiles and better insulin resistance markers.
Which strains, how much, and how long?
Research often uses single strains at clinical doses or multi-strain blends in the 109–1011 CFU daily range. Typical reassessment comes at 8–12 weeks.
Synbiotic approaches that add inulin-type fructans or GOS can boost fermentation and raise satiety hormones like GLP-1 and PYY.
- Single strain: targeted effect, easier to attribute results.
- Multi-strain: broader coverage, may suit tolerance needs.
- Track waist, fasting glucose, triglycerides, HDL, and appetite logs.
Realistic expectation: benefits are adjuncts to diet and activity and accrue over weeks. Those on high-fat diets may need more fibre and time. Contact Wellness Concept to tailor strain and dose to personal targets and timelines.
How Probiotics Work: From gut microbiota modulation to metabolic benefits
Microbial signals from the intestine act on hormones and the immune system to shape metabolic health. This section outlines how targeted supplements reshape the gut ecosystem and lower inflammation. The mechanisms often overlap and work best with a fibre-rich diet common to mindful Malaysian plates.
Reducing metabolic endotoxemia and improving gut permeability
Certain strains strengthen tight junctions and boost mucus, raising intestinal barrier resilience. Lower LPS leakage reduces systemic inflammation and helps curb insulin resistance.
Short-chain fatty acids, bile salt hydrolase, and energy homeostasis
Microbial fermentation yields short-chain fatty acids (acetate, propionate, butyrate) that tune appetite, energy use, and anti-inflammatory pathways. Bile salt hydrolase activity alters bile recycling and may influence cholesterol handling and lipid profiles.
Immune tone, GLP-1/GLP-2, and gut-brain signals
Microbes raise GLP-1 and GLP-2, which help appetite control and mucosal repair. Animal studies show Akkermansia muciniphila reduced endotoxemia and inflammation, while mixes like VSL#3 increased GLP-1 and improved glucose tolerance.
“Restoring barrier function is a key step to reduce chronic inflammation and improve outcomes.”
- Mechanisms: lower LPS, tighter junctions, SCFA signalling.
- Evidence: animal and some human trials show reduced central fat and steadier fasting glucose.
- Practical: combine strains with prebiotic fibres to reinforce effects.
| Mechanism | Primary Action | Day-to-day Outcome |
|---|---|---|
| Barrier repair | Stronger tight junctions, more mucus | Less endotoxemia, lower inflammation |
| SCFA production | Energy signalling and immune modulation | Steadier energy, improved glucose control |
| BSH activity | Bile deconjugation and cholesterol handling | Better lipid profile trends |
| Hormone release | GLP-1/GLP-2 elevation | Lower appetite, mucosal repair |
Short-Chain Fatty Acids: The acetate-propionate-butyrate triangle
Short-chain fatty acids sit at the crossroads between diet, gut microbes, and measurable health gains. They arise when non-digestible carbohydrates ferment in the gut and then act locally and systemically.
SCFAs and insulin sensitivity, adiposity, and gene expression
Acetate, propionate and butyrate are core metabolites that shape host energy use. They signal via GPCRs and alter gene expression, helping to raise insulin sensitivity and reduce adiposity.
Some SCFAs also enter host lipid and carbohydrate pools, so microbial activity directly feeds metabolism. Stable SCFA production tends to lower low-grade inflammation linked to metabolic syndrome.
Butyrate producers and intestinal barrier support
Butyrate acts through HDAC inhibition and GPCR activation to boost barrier repair and protective immunity. Key producers include Clostridium clusters IV/XIVa, Faecalibacterium prausnitzii, and Roseburia intestinalis.
Cross-feeding between bifidobacteria and these butyrate producers—promoted by ITF and AX/AXOS fibres—amplifies butyrate supply and raises Tregs and IL-10, cutting pro-inflammatory T cells.
| SCFA | Primary action | Food/fibre source | Day-to-day effect |
|---|---|---|---|
| Acetate | Substrate for peripheral tissues | Whole grains, fruit | Energy balance support |
| Propionate | Gluconeogenesis signal | Legumes, oats | Improved glucose handling |
| Butyrate | HDAC inhibition, barrier repair | Resistant starch, AXOS | Stronger gut barrier, less inflammation |
“Boosting butyrogenic pathways is a practical way to support insulin sensitivity and waist measures.”
Restoring the Intestinal Barrier: Tight junctions, mucus layer, and inflammation control
A healthy intestinal barrier keeps microbial signals in the lumen and stops harmful compounds reaching the bloodstream. Tight junction proteins such as claudins and occludin, plus a thick mucus layer, form the frontline between food, microbes, and circulation.
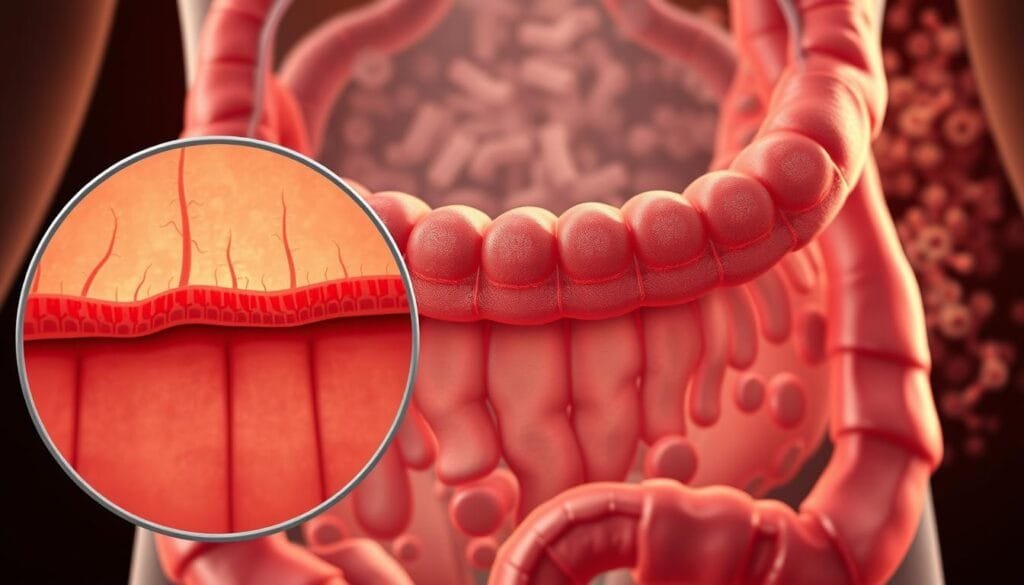
LPS entry into blood triggers endotoxemia. This raises inflammation and can worsen insulin resistance and other features of metabolic syndrome.
LPS, endotoxemia, and the metabolic cascade
LPS crossing the barrier sparks immune activation and chronic low-grade inflammation. This cascade harms glucose control and fat storage in adipose tissue.
Role of lactic acid bacteria and Akkermansia muciniphila
Lactic acid bacteria acidify the lumen and make bacteriocins that deter pathogens and support tighter junctions. Akkermansia muciniphila helps thicken mucus, lowers endotoxemia, and reduces adipose inflammation in human gut studies.
- Stress and high-fat diet weaken the barrier and raise gut permeability.
- GLP-2 and synbiotic approaches can improve sealing and reduce LPS leak.
- Signs of progress: less bloating, steadier energy, better fasting glucose.
| Barrier component | Primary role | Daily outcome |
|---|---|---|
| Tight junctions | Block paracellular leak | Lower endotoxemia, less inflammation |
| Mucus layer | Physical buffer to microbes | Reduced pathogen contact, improved repair |
| Commensal microbiota | Produce acids, SCFAs, and signals | Stronger barrier, steadier glucose |
“Restoring the barrier is foundational to long-term metabolic gains.”
Evidence Snapshot: From animal models to human randomized controlled trials
Clinical and animal research now links targeted gut interventions to measurable changes in fat distribution and metabolic markers. The following evidence highlights which strains showed benefits and how robust those effects were.
Weight and visceral fat gains seen with Lactobacillus gasseri LG2055
In a double-blind randomized controlled trial, adults who ate 200 g/day of fermented milk with LG2055 for 12 weeks cut visceral fat by ~4.6% and subcutaneous fat by ~3.3%.
They also saw reductions in body weight, BMI, waist, and hip. These changes matter because visceral fat predicts risk more than scale alone.
Insulin sensitivity and lipid improvements with Bifidobacterium
Clinical trials report that targeted Bifidobacterium lactis improved lipid profiles and cytokine patterns in people with metabolic syndrome. These controlled trial results suggest modest benefits to glucose handling and inflammation.
Meta-analyses and supporting animal data
Meta-analyses of probiotic supplementation report small but significant gains in cardio-metabolic risk factors. Animal studies add mechanism: VSL#3 raised GLP-1 and improved glucose tolerance, while L. rhamnosus GG reduced liver disease signals in rodents.
- Takeaway: strain specificity and duration are key to repeating trial effects.
- Look for labeled probiotic strains with clinical backing and pair intake with a fibre-rich diet.
Key Probiotic Strains linked to metabolic benefits
Several targeted bacterial strains show real potential to change abdominal fat, liver markers, and glycemia in clinical studies.
Lactobacillus rhamnosus, L. plantarum, L. gasseri
L. gasseri LG2055 reduced abdominal fat in human trials. L. rhamnosus GG showed liver‑fat protection in animal work. L. plantarum improved glycemia in women with metabolic concerns.
These lactic acid bacteria are common in fermented foods and supplements. Some formulas also include lactobacillus acidophilus.
Bifidobacterium highlights
B. longum and B. adolescentis cut weight gain and raised insulin sensitivity in animal studies. B. lactis was linked to better lipid profiles in clinical cohorts.
Akkermansia and next‑gen options
akkermansia muciniphila targets the mucus layer and barrier health. A proof‑of‑concept study found improved insulin sensitivity and liver enzymes in overweight adults.
- Check strain IDs (e.g., LG2055) — benefits are strain‑specific.
- Typical study doses range across 10⁹–10¹¹ CFU and come as capsules, fermented foods, or sachets.
- Pair strains with prebiotic fibres to boost colonization; expect variable individual responses based on baseline microbiota and diet.
Synbiotics 101: Pairing probiotics with prebiotics for stronger results
Pairing live cultures with selective fibres often produces larger shifts in gut signals than either alone. Synbiotics combine beneficial microbes and targeted fibres to boost colon activity and shape the intestinal microbiota.
Inulin-type fructans and GOS
ITF and GOS selectively feed Bifidobacterium, raising GLP-1 and PYY release. These peptide changes can help appetite control and small gains in waist and fasting glucose within weeks.
Arabinoxylan/AXOS and cross-feeding
AX and AXOS support Bifidobacterium and Roseburia, lowering endotoxemia in animal models. Cross-feeding converts acetate and lactate from bifidobacteria into butyrate via secondary degraders like Roseburia. That relay boosts short-chain fatty acids and supports barrier repair.
- Why synbiotics: fibres amplify live strain effects and sustain modulation gut activity.
- Start low and titrate to avoid gas; build fermentation capacity over days.
- Food-first options: onions, bananas, whole grains; add supplements as needed.
- Consistent daily intake is key to steady SCFA production and lasting changes gut microbiota.
Designing a Practical Protocol: Doses, duration, and combinations
A practical plan balances dose, timing, and diet to maximise measurable gains. This short protocol helps readers test targeted supplements while tracking key markers and comfort.
Single strain vs multi-strain: when to use which
Single, clinically-backed strains suit targeted goals when trials support a clear effect (eg, LG2055 at 12 weeks). Choose these when one endpoint is the priority.
Multi-strain blends like VSL#3 may give broader coverage and have shown prevention and treatment signals in obesity and type 2 diabetes models. Use blends when tolerance or multiple pathways are desired.
Timing with meals and course length
Start doses in study ranges (roughly 10⁹–10¹¹ CFU daily) and titrate for tolerance. Take supplements with meals to improve survival through the upper GI.
Run an initial 8–12 week course before judging outcomes. Pair with inulin-type fructans or other prebiotics from week one to boost GLP-1 and PYY effects.
- Check-in schedule: baseline, week 4, week 8, week 12 with agreed markers (waist, fasting glucose, lipids).
- If bloating occurs: lower dose, increase fluids, spread intake across the day.
- Rotate or layer strains if progress plateaus, keeping one core strain continuous.
- Avoid combining with antibiotics unless advised; adherence and diet determine most effect size.
“Consistent intake with a fibre-rich diet gives the best chance to repeat clinical effects.”
Personalization Factors: Diet, baseline microbiome, and lifestyle
Individual food choices and daily habits shape how well an intervention will alter the gut and its health signals. Tailoring plans to local Malaysian plates and routines improves early gains and long-term adherence.

High-fat diets, fiber gaps, and Malaysian food patterns
Western-style, high-fat diet and high-sugar patterns common in urban settings often lower fibre intake and shift key microbiota balances. This raises permeability, which allows LPS and other compounds to cross the barrier and spark inflammation.
Simple swaps — more legumes, leafy greens, and whole grains — help the gut ferment more fibre and support satiety hormone signals that reduce appetite and body weight over time.
Who may respond better—and how to track progress
People with higher baseline microbiome diversity tend to respond faster to modulation gut microbiota. Those with low diversity or long-term high-fat diet exposure may need longer courses and added prebiotic support.
- Track: waist, fasting glucose, TG/HDL, energy, and GI comfort.
- Reduce alcohol and added sugar modestly to lower barrier stress.
- Keep daily movement, sleep regularity, and stress management to support immune balance.
- Log stool timing and consistency as indirect markers of fermentation and effects.
Wellness Concept can help tailor plans and monitor changes to the gut microbiota and metabolic health.
Safety, Quality, and Regulatory Notes
Not all live culture products are created equal; careful selection matters for both safety and benefit. This short guide outlines what to check when choosing supplements aimed at the gut.
Strain identity, dose, and evidence
Strain-specificity is key: choose labeled strains with clinical backing rather than generic species names. Typical study doses range across 10⁹–10¹¹ CFU daily, but higher counts do not always mean better outcomes.
When to consult a professional
Most products have a favourable safety profile. Yet people who are immunocompromised, severely ill, pregnant, or on complex medications should consult a clinician first.
- Check third-party testing and transparent labels.
- Expect minor transient gas; reduce dose and build up slowly.
- lactobacillus acidophilus often appears in blends and should include strain ID.
- Store per label: refrigerated vs shelf-stable affects viability.
“Consistency and documented response give the best chance to gauge safety and effects.”
| Item | Why it matters | Practical tip |
|---|---|---|
| Strain ID | Determines clinical effects | Pick labeled strains with trials |
| CFU range | Matches trial doses | Follow study-equivalent amounts |
| Testing & storage | Ensures potency | Look for third-party seal; follow storage |
| Medical caution | Safety in vulnerable groups | Consult clinician before use |
Beyond the Capsule: Diet, exercise, and sleep synergy
Small daily habits—what someone eats, moves, and sleeps—shape how well gut-targeted plans work. Higher diet quality and lower saturated fat intake link to better control of body weight and metabolic markers in Malaysian adults.
Diet quality, saturated fat, and body weight management
Moderating saturated fat and boosting whole-food fibers shifts fermentation toward healthful short-chain fatty acids. This supports insulin action and lowers inflammation.
Regular movement improves insulin sensitivity and raises microbial diversity, while consistent sleep helps appetite hormones and barrier repair. Hydration aids motility and metabolite clearance.
Building a gut-friendly plate that supports probiotic effects
A simple plate: diverse plants, lean proteins, and fermented foods. Add prebiotic fibres to raise GLP-1 and PYY and tune satiety cues.
- Encourage weekly meal rhythms to stabilise the gut-brain axis and microbiome.
- Lactic acid produced by lactic acid bacteria inhibits pathogens and supports peristalsis.
- Combine mindful eating, hydration, and movement to double the supplements’ effects.
“Lifestyle synergy often doubles the gains seen from supplements alone.”
Real-World Outcomes: Body weight, insulin resistance, and liver health
Evidence from humans and animals ties gut modulation to changes in body shape, insulin action, and liver outcomes.
Visceral fat, NAFLD links, and lipid metabolism
One randomized controlled study with LG2055 reported reduced visceral fat and lower body weight after 12 weeks. Animal work with L. rhamnosus GG showed protection against nonalcoholic fatty liver disease, highlighting hepatic benefits seen in models.
Bifidobacterium spp. has been tied to better insulin resistance and improved lipid profiles via bile salt hydrolase activity and lower endotoxemia.
Markers to monitor: glucose, TG/HDL, waist, inflammatory biomarkers
Track fasting glucose, TG/HDL ratio, waist circumference, and simple inflammatory markers across a 12-week window. Waist measures often change before total body fat or scale weight, so they act as an early, sensitive indicator.
Pair objective metrics with how someone feels: energy, satiety, and GI comfort. Controlled trial data and clinical experience show gradual, sustained change beats rapid shifts. Seek ongoing review and adjust plans with a clinician to support long-term diabetes and metabolic syndrome risk reduction.
Speak to Wellness Concept in Malaysia
Contacting Wellness Concept begins with a short message to review goals and local routines. The team turns clinical evidence into a clear plan that suits Malaysian plates and daily life.
WhatsApp: +60123822655
Business hours
Monday–Friday 9:30 am–6:30 pm; Saturday 10 am–5 pm; Sunday Closed.
How they guide strain selection, synbiotic plans, and follow-up
Personalised matching: the team maps clinically studied probiotic strains such as L. gasseri LG2055, B. lactis, and L. rhamnosus GG to goals like visceral fat reduction and glycemic control.
- Design synbiotic plans using ITF, GOS or AX/AXOS while monitoring tolerance.
- Set a clear timeline with check-ins at weeks 4, 8, and 12 and agreed markers: waist, fasting glucose, and lipids.
- Advise on diet changes that support colonization and steady SCFA production.
- Explain labels, CFU counts, storage, and quality assurance to ensure product value.
- Coordinate with healthcare providers and adjust protocols if side effects arise.
Education and support continue beyond the initial course. They help interpret changes, sustain adherence, and review long-term effects of probiotic supplementation while prioritizing comfort and safety.
Readers may also explore how to find gut inflammation relief with tailored guidance from Wellness Concept.
“Personalised plans that pair clinical strains with targeted fibres give the best chance to repeat trial effects.”
Conclusion
A gut-focused plan can add measurable gains to weight, blood sugar, and lipid control when paired with lasting diet and lifestyle change.
Probiotics taken consistently, with strain-specific choice, may deliver meaningful beneficial effects by helping repair the barrier, boosting short-chain fatty acid production, and lowering endotoxemia. Synbiotics and next-generation options broaden practical choices and often amplify results when meals are fibre-rich.
Evidence supports modest reductions in visceral fat, improved glycemia, and better lipids over weeks to months. Personalization matters: baseline microbiota, daily routine, and food habits shape outcomes. Track waist, fasting glucose, and tolerance, then revisit strain choice and dosing as needed.
Wellness Concept in Malaysia can help set a structured, measurable plan. WhatsApp +60123822655 to begin a tailored program and start steady progress.
FAQ
What is the link between gut microbiota and metabolic health?
The community of microbes in the intestinal microbiota influences inflammation, energy harvest, and gut permeability. Imbalances can raise circulating LPS, drive low-grade inflammation, and worsen insulin resistance, body weight, and lipid profiles. Modulating the gut ecosystem can reduce endotoxemia and support metabolic improvements.
Can lactic acid bacteria and other strains help reduce body fat or waist circumference?
Certain strains such as Lactobacillus gasseri and some Bifidobacterium species have been associated in clinical trials with modest reductions in visceral fat and body weight. Effects are strain-specific and usually small to moderate, so they work best alongside diet and exercise.
Which strains show the strongest evidence for improving insulin sensitivity?
Trials point to combinations including Bifidobacterium longum, B. lactis, and Lactobacillus plantarum or rhamnosus as beneficial for glycemic control and insulin sensitivity. Akkermansia muciniphila shows promising results as a next‑generation candidate but is less widely available in supplements.
How do short-chain fatty acids (SCFAs) like acetate, propionate, and butyrate affect metabolism?
SCFAs produced by fiber-fermenting microbes regulate energy homeostasis, modulate GLP-1/GLP-2 secretion, improve insulin sensitivity, and strengthen the intestinal barrier. Butyrate also supports epithelial health and reduces inflammation.
What dose and duration are typically used in randomized controlled trials?
Many studies use daily doses in the range of 1–10 billion to over 100 billion CFU, often for 8–24 weeks. Benefits depend on strain, dose, and baseline status; multi-strain products sometimes outperform single strains for complex outcomes.
Should synbiotics be preferred over single strains?
Combining prebiotics like inulin-type fructans or GOS with targeted microbes can enhance bifidogenic and butyrogenic pathways via cross-feeding. Synbiotics often improve colonization and SCFA production, but product formulation and evidence should guide choice.
Are there safety concerns or people who should avoid supplementation?
Most healthy adults tolerate supplements well. People with severe immunosuppression, critical illness, or certain central venous catheters should consult a clinician. Quality, strain specificity, and manufacturing standards are important for safety and efficacy.
How quickly might someone see changes in markers like fasting glucose or triglycerides?
Some trials report early shifts in inflammatory markers and gut permeability within weeks, while measurable changes in fasting glucose, TG/HDL ratio, or weight commonly appear after 8–12 weeks. Consistency, diet quality, and activity level affect outcomes.
What role does diet play alongside microbial interventions?
Diet is crucial. High-fiber patterns promote SCFA-producing bacteria, while high-fat, low-fiber diets favor dysbiosis. A gut-friendly plate rich in whole grains, legumes, fruits, and vegetables enhances the effects of targeted microbial therapies.
How can a person track whether an intervention is working?
Useful markers include waist circumference, body composition or visceral fat (if available), fasting glucose and insulin, HbA1c, lipid panels, and inflammatory biomarkers such as CRP. Symptom tracking and follow-up consultations help personalize adjustments.
Is there evidence that microbial modulation helps nonalcoholic fatty liver disease (NAFLD)?
Emerging trials indicate that certain strains may reduce liver fat and improve lipid metabolism and inflammatory markers. Effects vary and are generally greater when combined with weight loss and dietary change.
How should consumers choose a high-quality product?
Look for products with clinically studied strains, clear CFU counts at expiry, third-party testing, and transparent manufacturing. Prefer formulations tied to randomized controlled trials relevant to glucose, weight, or lipid outcomes.
Do Malaysian dietary patterns affect response to microbial therapies?
Regional diets influence baseline microbiome composition. High intake of refined carbohydrates, saturated fat, or low fiber may blunt response, while increasing local fiber-rich foods and fermented items supports colonization and SCFA production.
Can microbial interventions replace medications for type 2 diabetes or dyslipidemia?
They are adjunctive, not replacements. Evidence supports modest improvements in insulin sensitivity and lipids, but they should complement prescribed therapies and lifestyle modification under medical guidance.
How do gut permeability and tight junctions relate to treatment effects?
Strengthening tight junctions and mucus supports the barrier against LPS translocation. Certain lactic acid bacteria and butyrate-producing species promote junctional protein expression and mucus layer integrity, reducing metabolic endotoxemia.
Where can people in Malaysia get personalized advice from Wellness Concept?
Wellness Concept offers guidance on strain selection, synbiotic plans, and follow-up via WhatsApp at +60123822655 during business hours: Mon–Fri 9:30 am–6:30 pm and Sat 10 am–5 pm. They tailor protocols to diet, baseline microbiome, and lifestyle.



